Cardiovasc Diabetol:与阿托伐他汀和瑞舒伐他汀相比,匹伐他汀对新发糖尿病的影响
2022-06-13 从医路漫漫 MedSci原创
匹伐他汀是一种与阿托伐他汀和瑞舒伐他汀并驾齐驱的高效他汀类药物。

背景:他汀类药物降低血胆固醇水平,广泛用于心血管疾病的一级或二级预防。虽然他汀类药物治疗通常被认为是安全的,但最近的几项研究表明,它会增加新发糖尿病的风险(NODM) 。总的来说,他汀类药物会增加10-12%的NODM风险,高强度他汀类药物治疗的风险略高于低强度或中等强度治疗。然而,由于直接比较他汀类药物的数据有限,单个他汀类药物的NODM风险仍然存在争议。先前的荟萃分析显示,不同他汀类药物之间的糖尿病风险没有显著差异,而一项基于人群的回顾性队列研究显示,与普伐他汀相比,阿托伐他汀和辛伐他汀与NODM风险增加相关。此外,Yoon等人报道,在各种他汀类药物中,与匹配的非暴露队列相比,暴露于阿托伐他汀的队列具有最高的NODM风险。相反,一项对17项研究的荟萃分析报告称,在各种他汀类药物中,瑞舒伐他汀与NODM风险最相关。
匹伐他汀是一种与阿托伐他汀和瑞舒伐他汀并驾齐驱的高效他汀类药物。服用匹伐他汀4 mg后,低密度脂蛋白胆固醇平均下降47%,与阿托伐他汀40 mg或瑞舒伐他汀10 mg相当。先前的随机临床试验表明,与1 mg治疗相比,匹伐他汀 4 mg治疗显著降低了低密度脂蛋白胆固醇和临床结果,而与肾功能状态无关。当联合使用匹伐他汀和培马贝特时,改善高血压和胰岛素抵抗模型大鼠的血脂状况和内皮功能。IHM等人。也有报道称,在心血管疾病高危患者中,与单用匹伐他汀相比,联合应用匹伐他汀和非诺贝特能更有效地降低非高密度脂蛋白胆固醇。先前的几项研究已经报道,与普伐他汀、阿托伐他汀或瑞舒伐他汀等其他他汀类药物相比,匹伐他汀对糖尿病的发展或糖代谢的影响较小。此外,在一项针对亚洲患者的真实队列研究中,比起其他他汀类药物,匹伐他汀对NODM的风险比(HR)略低。相比之下,一项包括3680名患者的单中心回顾性研究报告称,比起其他他汀类药物,匹伐他汀与NODM的相关性更强。这些不确定的结果可能是由于用于单个他汀类药物直接比较的数据有限和各种偏差,包括选择、不朽、原始和/或源于研究设计错误、相对较小的样本量或分析方法的混杂偏差。
目的:在目前的新用户模型队列研究中,我们使用观察性医疗结果伙伴关系(OMOP)-公共数据模型(CDM)评估了在没有糖尿病或糖耐量受损的患者中,匹伐他汀与世界上最常用的他汀类药物阿托伐他汀或瑞舒伐他汀对NODM的影响,这些数据在我们之前的研究中得到了验证
方法:将来自10家医院的电子健康记录数据转换为观察医疗结果伙伴关系公共数据模型(n = 14,605,368例患者),用于识别新服用匹伐他汀、阿托伐他汀或瑞舒伐他汀(阿托伐他汀+瑞舒伐他汀)达≥ 180天且既往无糖尿病史或HbA1c水平≥ 5.7%的患者。我们采用Cox回归分析进行了一项队列研究,以检查倾向评分匹配(PSM)后NODM的风险比(HR ),然后对HR进行了汇总荟萃分析。
结果:在1:2 PSM后,从10个数据库中汇集了10,238名新的匹伐他汀使用者(15,998人年随访)和18,605名阿托伐他汀+罗苏伐他汀使用者(33,477人年随访)。对风险比的荟萃分析表明,与阿托伐他汀+罗苏伐他汀相比,匹伐他汀导致NODM风险显著降低(风险比0.72;95%可信区间为0.59–0.87)。在亚分析中,在1:1 PSM后,匹伐他汀与阿伐他汀或罗苏伐他汀相比,与较低的NODM风险相关(HR 0.69置信区间0.54–0.88,风险比0.74;置信区间分别为0.55-0.99)。与低至中等强度的阿托伐他汀+罗苏伐他汀使用者相比,匹伐他汀使用者发生NODM的风险始终较低(HR 0.78置信区间0.62–0.98)。
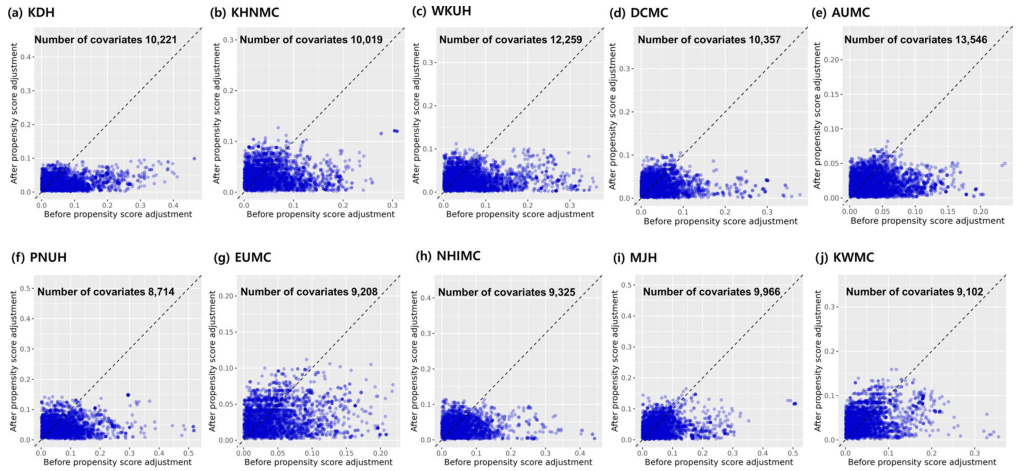
图1 10个数据库倾向得分匹配前后的协变量平衡图
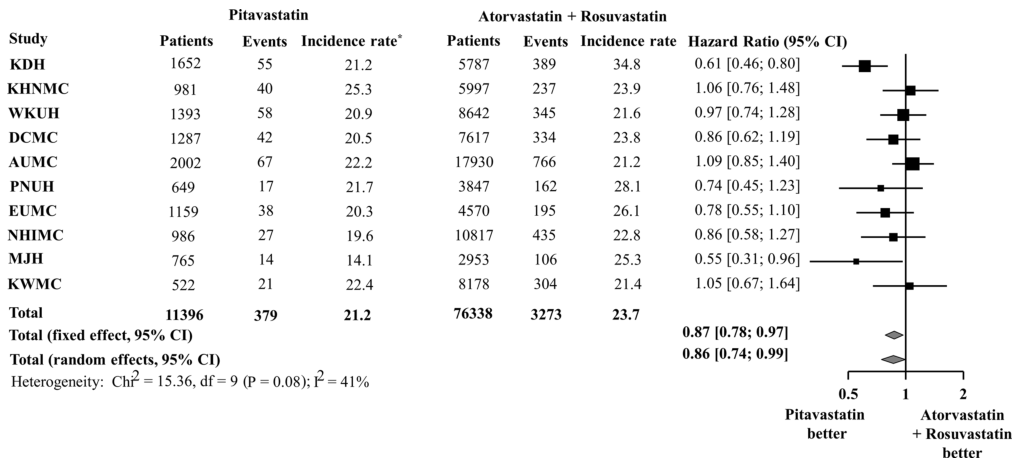
图2在总体人群中,匹伐他汀与阿托伐他汀或瑞舒伐他汀相比新发糖尿病的风险。*每千人年发病率
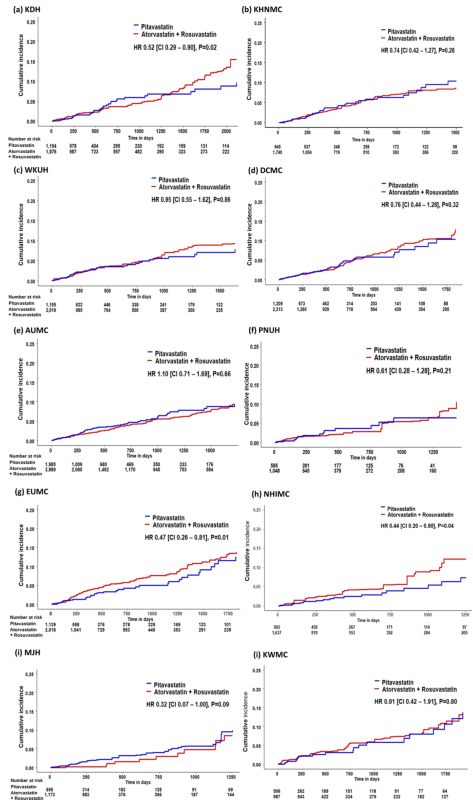
图3 Kaplan-Meier图比较了倾向得分匹配后10个数据库中匹伐他汀与阿托伐他汀或瑞舒伐他汀治疗新发糖尿病的风险
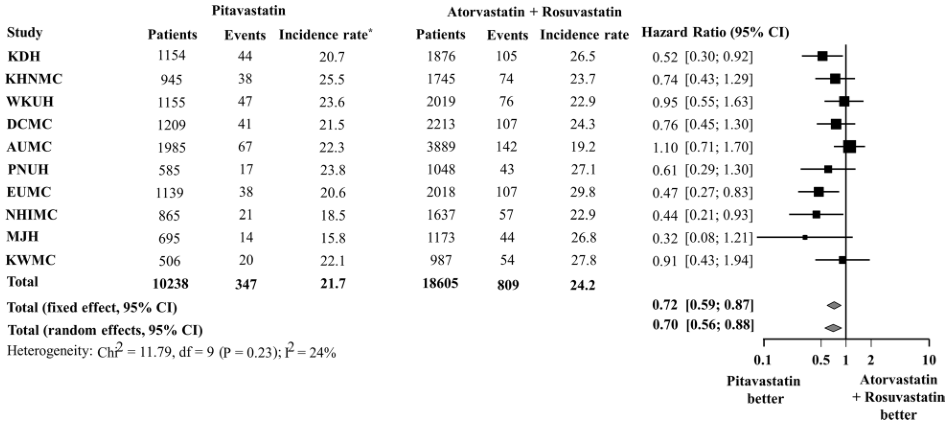
图4倾向评分匹配后,匹伐他汀与阿托伐他汀或瑞舒伐他汀之间新发糖尿病的风险。*每千人年发病率

图5 1:1倾向评分匹配后新发糖尿病的风险。A比阿托伐他汀,B比瑞舒伐他汀,C阿托伐他汀比瑞舒伐他汀。*每千人年发病率
结论:在这项回顾性、多中心、主动比较、新用户、队列研究中,与阿托伐他汀或瑞舒伐他汀相比,匹伐他汀降低了NODM的风险。
原文出处:Seo WW, Seo SI, Kim Y,et al.Impact of pitavastatin on new-onset diabetes mellitus compared to atorvastatin and rosuvastatin: a distributed network analysis of 10 real-world databases.Cardiovasc Diabetol 2022 05 23;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BET#
50
#ASC#
44
#DIA#
42
#匹伐他汀#
56