Cardiovasc Diabetol:不同他汀类药物对新发糖尿病风险的影响
2022-05-28 MedSci原创 MedSci原创
与阿托伐他汀或瑞舒伐他汀相比,匹伐他汀可降低新发糖尿病风险
他汀类药物可有效降低血胆固醇水平,被广泛用于心血管疾病的一级或二级预防。尽管他汀类药物治疗通常被认为是安全的,但最近的几项研究表明,它会增加新发糖尿病 (NODM) 的风险。
然而,目前直接比较单个他汀类药物的 NODM 风险的数据有效。本文使用可靠的大规模数据比较了使用匹伐他汀(pitavastatin)和阿托伐他汀(atorvastatin)或瑞舒伐他汀(rosuvastatin)的患者的 NODM 风险。
研究人员将十家医院的电子健康记录数据转换成观察性医疗结局合作伙伴通用数据模型,用以筛查至少6个月内没有糖尿病病史、且糖化血红蛋白浓度<5.7%的匹伐他汀、阿托伐他汀或瑞舒伐他汀(阿托伐他汀+瑞舒伐他汀)的新服用者。研究人员使用 Cox 回归分析进行了一项队列研究,以检查倾向评分匹配 (PSM) 后 NODM 的风险比 (HR),然后对 HR 进行汇总荟萃分析。
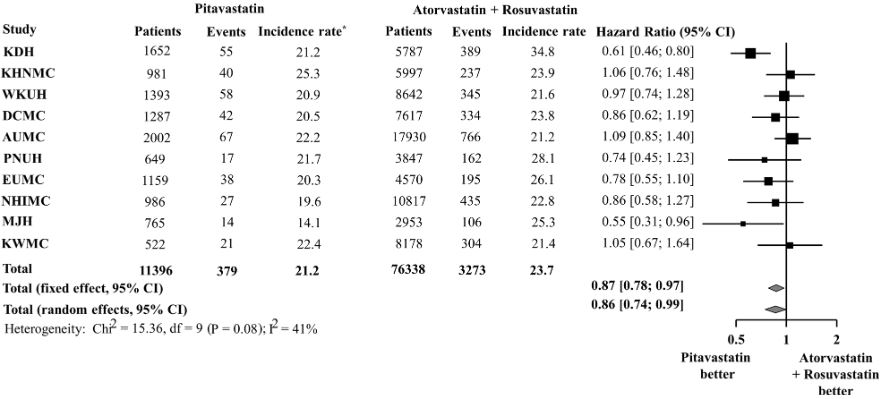
10个数据库不同他汀类药物服用者的新发糖尿病风险
经1:2倾向评分匹配后,从10个数据库中共汇集了10238位匹伐他汀新服用者(随访了15998个人·年)、18605位阿托伐他汀+瑞舒伐他汀新服用者(随访了33477个人·年)。HR 的荟萃分析表明,与阿托伐他汀+瑞舒伐他汀相比,匹伐他汀可显著降低服用者的 NODM 风险(HR 0.72)。
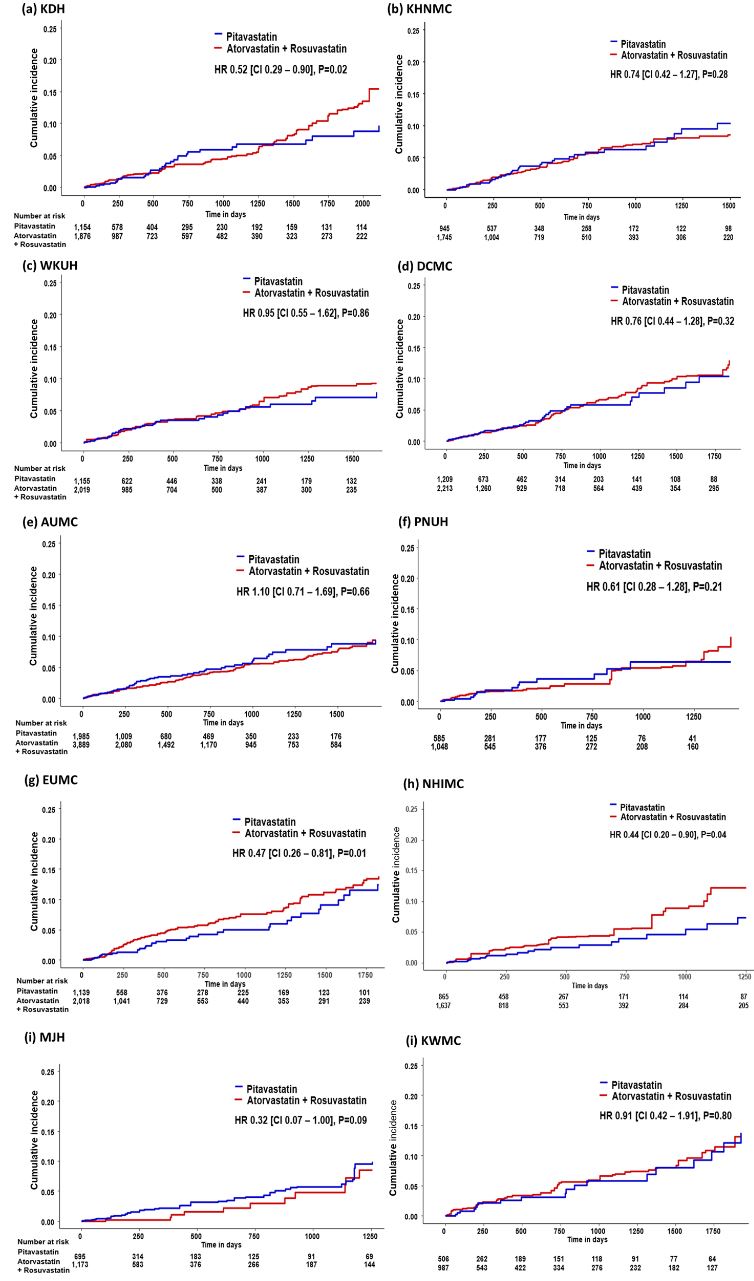
10个数据库不同他汀类药物服用者的新发糖尿病的累积发生率
在亚组分析中,经1:1倾向评分匹配后,与阿托伐他汀或瑞舒伐他汀相比,匹伐他汀与服用者的 NODM 风险降低相关(HR分别是0.69和0.74)。与低至中等强度阿托伐他汀+瑞舒伐他汀服用者相比,匹伐他汀服用者的 NODM 风险始终较低(HR 0.78)。
综上,在这项回顾性、多中心队列研究中,与阿托伐他汀或瑞舒伐他汀相比,匹伐他汀可降低新发糖尿病风险。
原始出处:
Seo, WW., Seo, S.I., Kim, Y. et al. Impact of pitavastatin on new-onset diabetes mellitus compared to atorvastatin and rosuvastatin: a distributed network analysis of 10 real-world databases. Cardiovasc Diabetol 21, 82 (2022). https://doi.org/10.1186/s12933-022-01524-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#ASC#
33
#他汀类药#
56
#DIA#
36
#BET#
29
确定没被充值就好啊
28
学习了
52