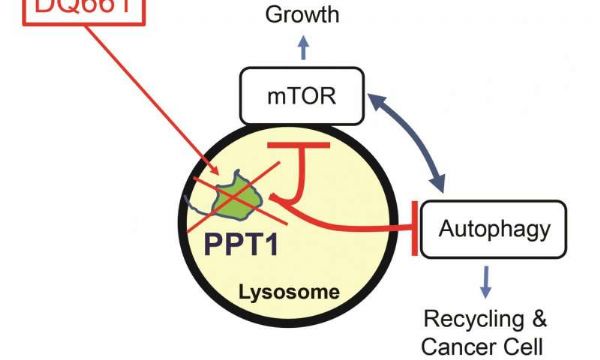
Cancer Discovery:研究人员确定靶点“PPT1”,为癌症患者带来了希望
2017-09-21 佚名 medicalxpress
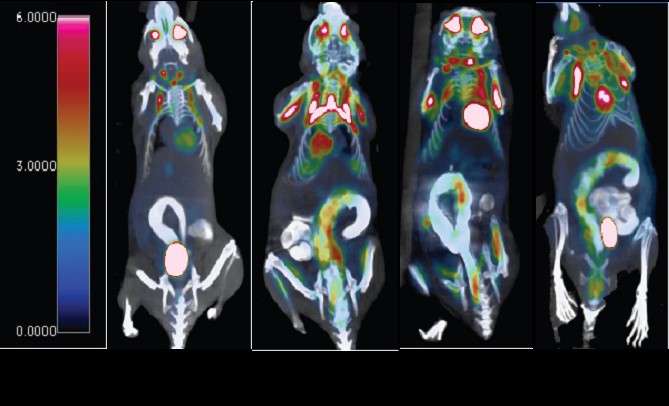
宾夕法尼亚大学(UniversityofPennsylvania)的研究人员开辟了一条与癌症抗争的新途径,他们找到了一种方法来锁定一种对肿瘤生长至关重要的酶,同时也阻断了过去试图将这种酶用于治疗的机制。研究人员能够利用这一发现开发出一种药物,成功地抑制了黑色素瘤的生长,以及在小鼠体内的胰腺和结直肠癌。《癌症研究》杂志本月在网上公布了这一发现。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#cover#
60
#Dis#
26
#PPT#
39
#研究人员#
23
学习了.谢谢分享
53
#癌症患者#
26
#ISC#
38