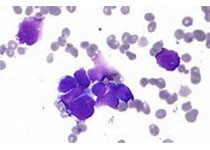
Blood:结合初始和诱导后PET,建立更为准确的预测滤泡性淋巴瘤患者预后的模型
2018-03-21 MedSci MedSci原创
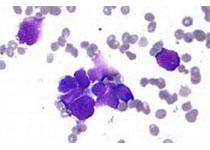
根据基线PET计算的总代谢肿瘤体积(TMTV)和诱导结束后的PET(EOI PET)均是成像生物标志物,可提示高肿瘤负荷的滤泡性淋巴瘤患者早期危险分层的前景。近日,Blood上发表一篇文献,Anne Ségolène Cottereau等人结合来159位患者(源于3个前瞻性试验)的这两个数据,建立了一相关模型。对于这159位患者,中位随访64个月。高TMTV(>510cm3)和EOI PET
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#患者预后#
26
#PE#
28
谢谢分享.学习了
58
#滤泡性淋巴瘤#
34
#PET#
29
学习
1