Blood:FOXP1表达可作为预测利妥昔单抗治疗滤泡性淋巴瘤预后的标志物。
2017-11-20 MedSci MedSci原创
滤泡性淋巴瘤(FL)是一种在临床上和分子上都具有高度异质性的疾病,目前预测主要是依赖于临床检验。研究人员近期发现7个基因(包括EZH2和MEF2B)突变状态的综合,会提高风险分层。研究人员收集基因表达数据来揭示在EZH2和MEF2B突变的病例中的差异性表达的基因。经过筛查,研究人员集中于FOXP1基因,运用免疫组化(IHC)检测763份组织样本FOXP1蛋白的表达量。为了结果的相关性,纳入了一个包
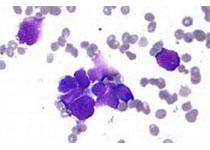
滤泡性淋巴瘤(FL)是一种在临床上和分子上都具有高度异质性的疾病,目前预测主要是依赖于临床检验。研究人员近期发现7个基因(包括EZH2和MEF2B)突变状态的综合,会提高风险分层。研究人员收集基因表达数据来揭示在EZH2和MEF2B突变的病例中的差异性表达的基因。
经过筛查,研究人员集中于FOXP1基因,运用免疫组化(IHC)检测763份组织样本FOXP1蛋白的表达量。为了结果的相关性,纳入了一个包含142名用R-CVP治疗的FL患者队列,和一个包含395名用CHPOP+/-利妥昔单抗治疗的临床试验。经分析发现,FOXP1在EZH2和MEF2B突变的病例中均有显著下调。根据IHC,队列中有76例样本(54%)FOXP1高表达(>10%),恰好与五年正常存活(FFS)率下降相关(55% vs 70%)。在临床试验的队列中,248名(63%)患者FOXP1高表达,与接受R-CHOP的患者FFS显著缩短相关(HR 1.95,P=0.017),但与接受CHOP的患者无明显关联(HR 1.15,P=0.44)。对接受免疫化疗的患者,FOXP1高表达对FFS的影响是额外的。FOXP1高表达与特定的分子特征相关,如TP53突变、IRF4表达和暗区生殖中心或活化的B细胞的基因表达标记。
总而言之,FOXP1是基因突变的下游共性表型,可用于预测包含利妥昔单抗治疗方案的预后。
原始出处:
Anja Mottok, et al.FOXP1 expression is a prognostic biomarker in follicular lymphoma treated with rituximab-containing regimens.Blood 2017 :blood-2017-08-799080; doi: https://doi.org/10.1182/blood-2017-08-799080
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#利妥昔#
28
#标志物#
39
#滤泡性淋巴瘤#
45
学习了
66