ASCO 男性乳腺癌的管理 2020
Management of Male Breast Cancer
2020-02-01
目的 制定有关男性乳腺癌治疗的建议。
方法 ASCO召集了一个专家小组,根据系统的审查和正式的共识程序制定建议。
结果 26项描述性报告或观察性研究符合资格标准,并为建议提供了证据基础。
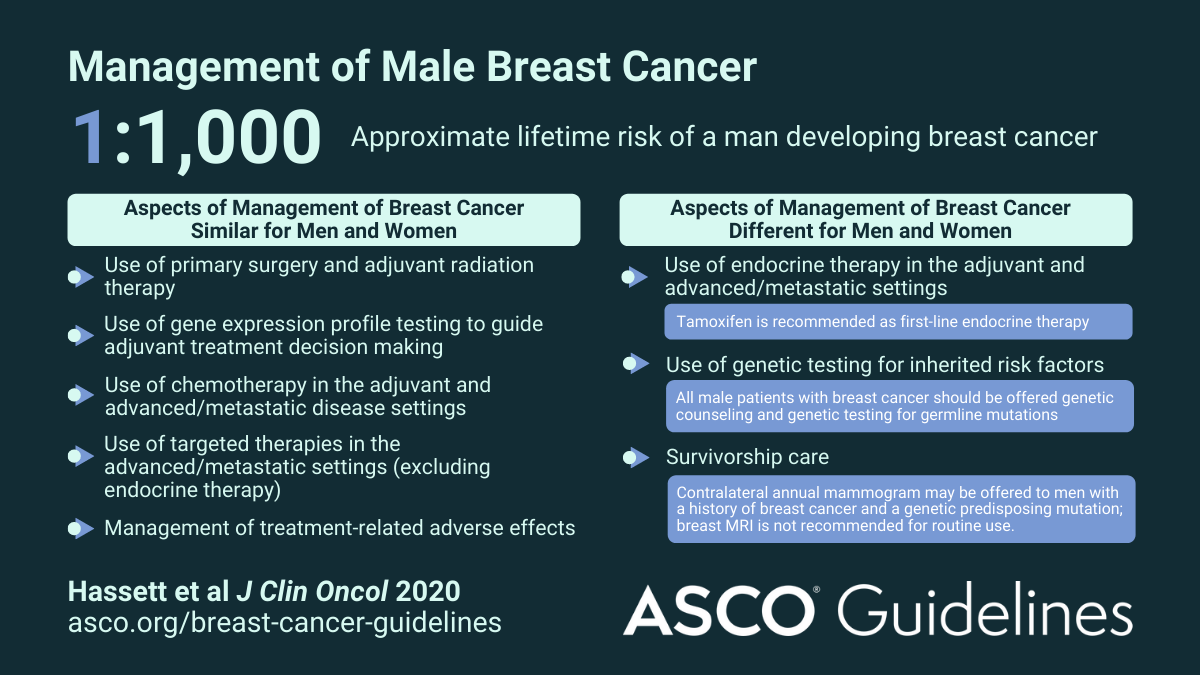
推荐建议 男性乳腺癌患者使用的许多管理方法与女性乳腺癌一样。接受辅助内分泌治疗的荷尔蒙受体阳性乳腺癌男性应开始接受他莫昔芬治疗,初始持续时间为五年;那些对他莫昔芬禁忌症的人可以给予促性腺激素释放激素激动剂/拮抗剂和芳香酶抑制剂。已完成他莫昔芬五年,耐受治疗且仍具有高复发风险的男性,可以再接受五年治疗。患有早期疾病的男性不宜使用骨修饰剂预防复发,但仍可以接受这些药物预防或治疗骨质疏松症。对于患有晚期或转移性疾病的男性,应给予内分泌治疗作为一线治疗,但内脏危机或快速进行性疾病除外。有针对性的全身疗法可用于治疗晚期或转移性癌症,使用与女性相同的适应症和组合。不论遗传因素如何,均应向有乳房切除术治疗史的男性患者提供同侧年度乳房X线照片;有乳腺癌病史和遗传易感性突变的男性,可以提供每年的对侧乳房X线照片。不建议常规进行乳房磁共振成像。应向所有患有乳腺癌的男性提供癌症易感基因的遗传咨询和种系遗传测试。








感谢
69
i
52
#学习#
53
非常感谢
75
发病率导致
76