CSCO 2011:FXR及其相关基因与原发性肝癌临床预后的相关性研究
2011-09-15 MedSci原创 MedSci原创
浙江大学医学院附属邵逸夫医院肿瘤内科 孙鹏 王凯峰 楼芳 潘宏铭 目的:在对原发性肝癌的研究中,寻找其有效的预后预测因子对于评估肝癌的病情及制定有效的治疗方案具有重要意义。核受体FXR(farnesoid X recePtor,FXR)能抑制肝脏肿瘤的形成。本文拟通过检测FXR及其下游基因MDR3、MRP在原发性肝癌组织中的表达,分析多种
浙江大学医学院附属邵逸夫医院肿瘤内科 孙鹏 王凯峰 楼芳 潘宏铭
目的:在对原发性肝癌的研究中,寻找其有效的预后预测因子对于评估肝癌的病情及制定有效的治疗方案具有重要意义。核受体FXR(farnesoid X recePtor,FXR)能抑制肝脏肿瘤的形成。本文拟通过检测FXR及其下游基因MDR3、MRP在原发性肝癌组织中的表达,分析多种影响因子同原发性肝癌病人的临床预后之间的关系,以期寻找并发现对临床实践有指导意义的预后因素。
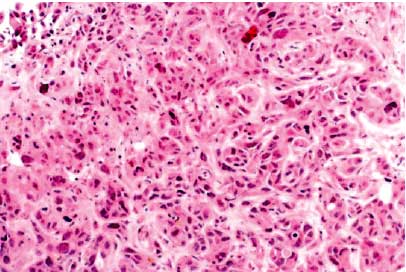
方法:收集26例原发性肝癌患者的手术切除肝癌组织,通过荧光定量RT-PCR检测FXR、MDR3以及MRP在肝癌组织中的表达;同时对上述 26名患者进行生存随访获取生存资料,通过病历查找获取患者的肿瘤特征、手术前后甲胎蛋白、总胆汁酸(TBA)、总胆红素(TB)、直接胆红素(CB)等的检验值。根据FXR、MDR3和MRP的表达水平和肝癌侵袭程度、甲胎蛋白、血清标志物(总胆汁酸、胆红素)进行生存分析,分别描绘KaPlan- Meier生存曲线,并对以上因素进行COX回归分析。本研究还进一步根据侵袭潜能联合基因表达水平对全组26例患者进行了亚组分层的生存分析。
结果:全组26名原发性肝癌患者的1年、2年和5年生存率分别为58%、38%和7%。FXR高表达组的中位总生存期为26.80个月,显著长于低表达组的7.27个月(P<0.05)。FXR高表达组的1年生存率、2年生存率分别为77%和53%,而FXR低表达组的1年生存率、2年生存率分别为38%和23%。手术后总胆红素升高组的中位生存期10.73个月,显著低于降低组的27.27个月(P<0.05)。肝细胞癌组的分析中,FXR高表达组的中位生存期26.80个月,显著高于低表达组的6.97个月(P<0.05)。亚组生存分析发现,FXR高表达联合低侵袭组有较好的生存预后,中位生存期为27.27个月,好于其它3个亚组(P<0.05)。对全组患者和肝细胞癌组患者进行了的COX回归分析表明,FXR的表达均是独立的预后因素 (P<0.05),而TBA的变化和MRP的表达分别是原发性肝癌和肝细胞癌的独立预后因素(P<0.05)。
结论:肝癌组织中FXR高表达、术后胆红素降低及低侵袭性的患者具有较好的临床预后,提示FXR表达的差异和临床预后有着密切的联系。FXR的表达联合肝癌侵袭程度分析能预测原发性肝癌患者的临床预后,可能是原发性肝癌治疗的预后因子之一。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#相关性#
44
#相关基因#
44
#原发性#
42
#原发性肝癌#
46
#临床预后#
43
#FXR#
41