高血压急症如何处理?来看最新中国专家共识!
2022-04-27 中华高血压杂志 中华高血压杂志
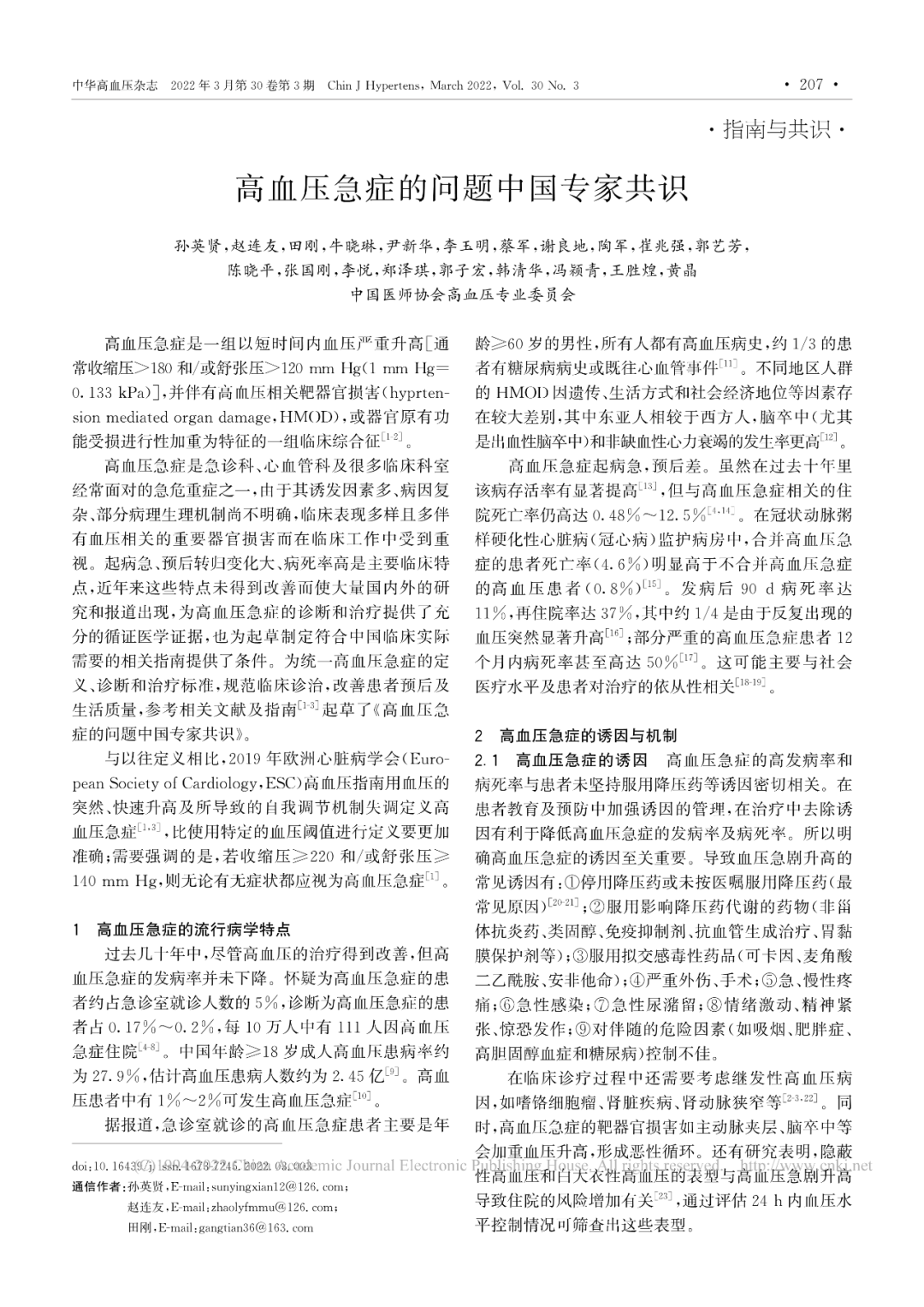
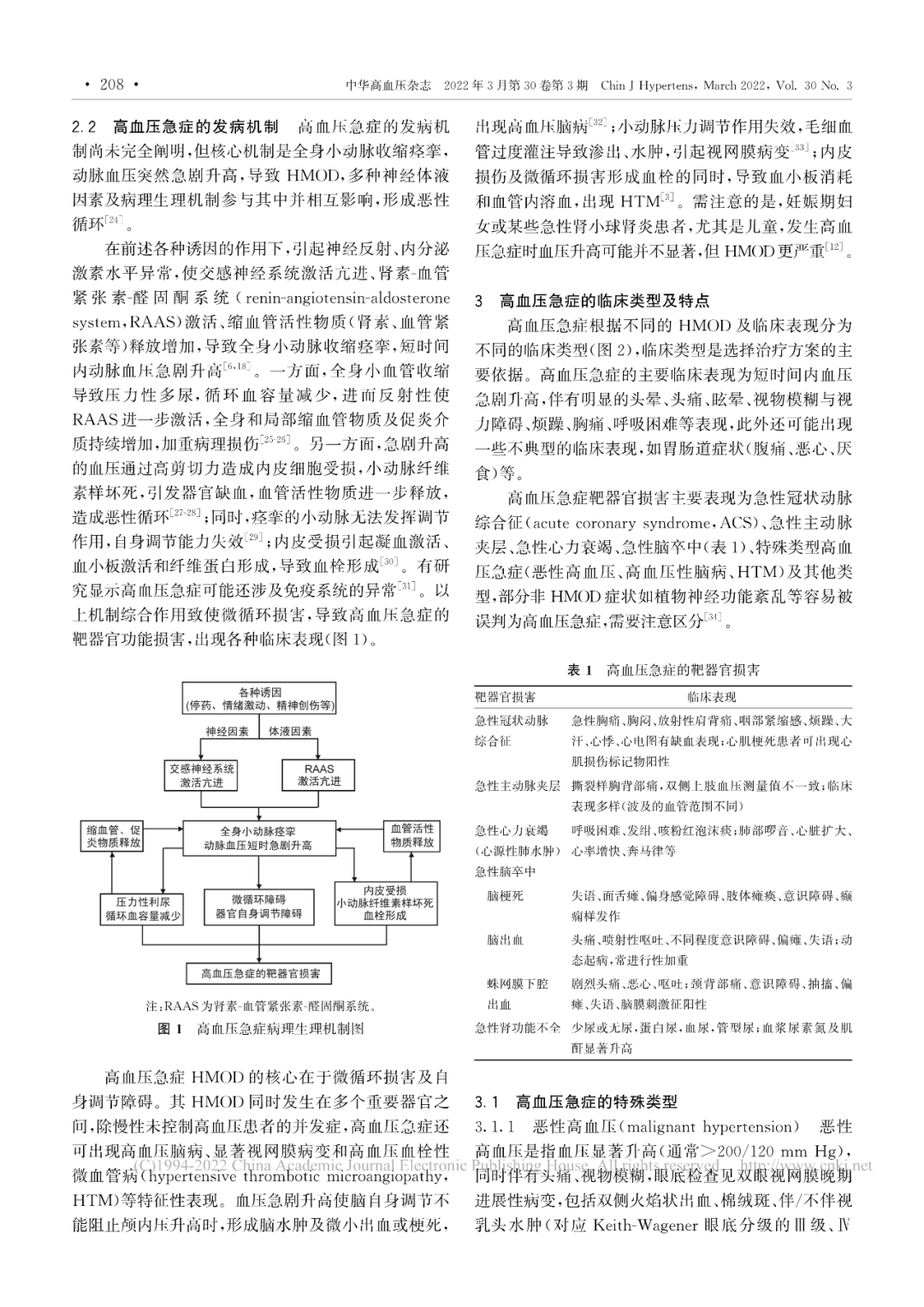
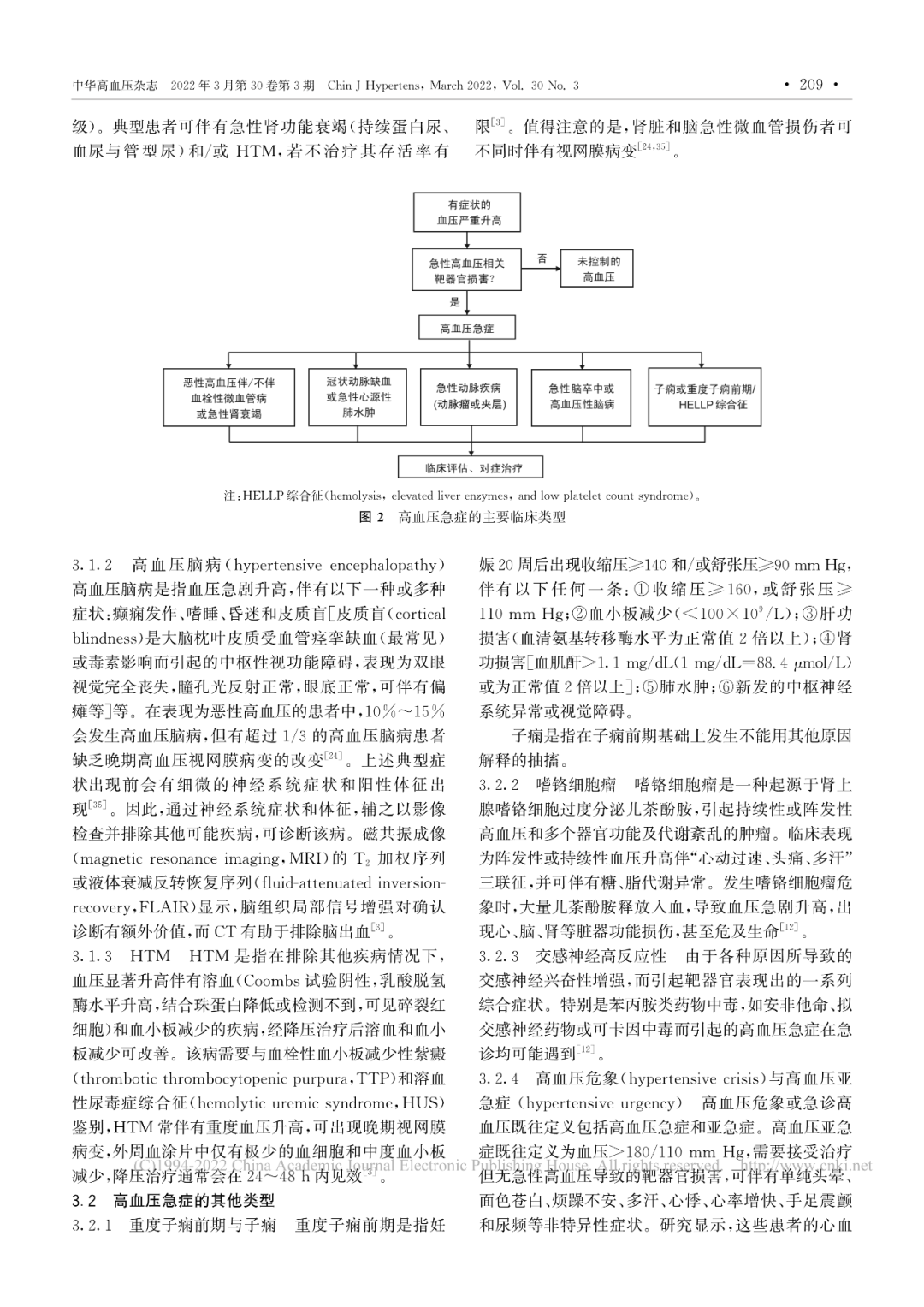
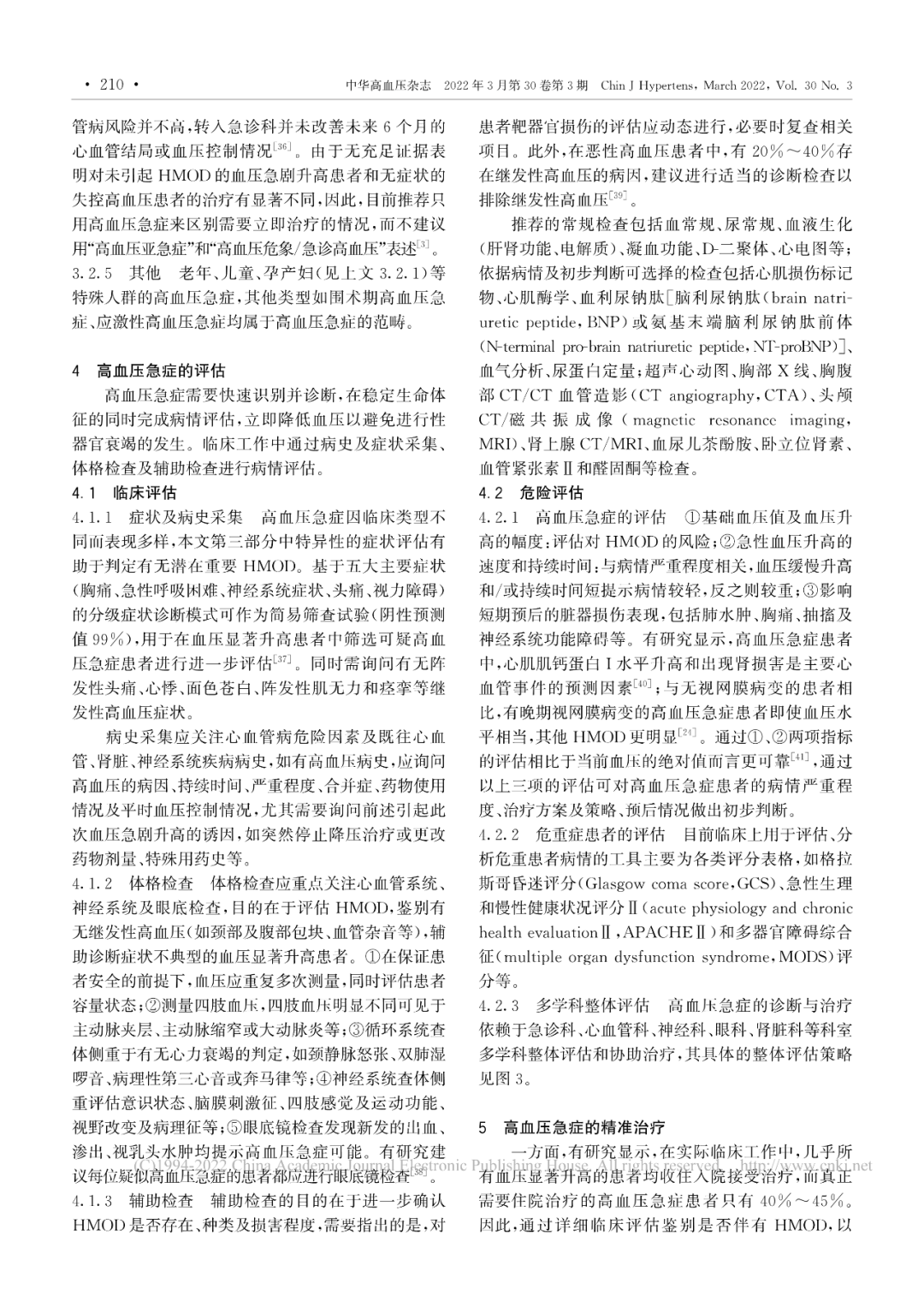
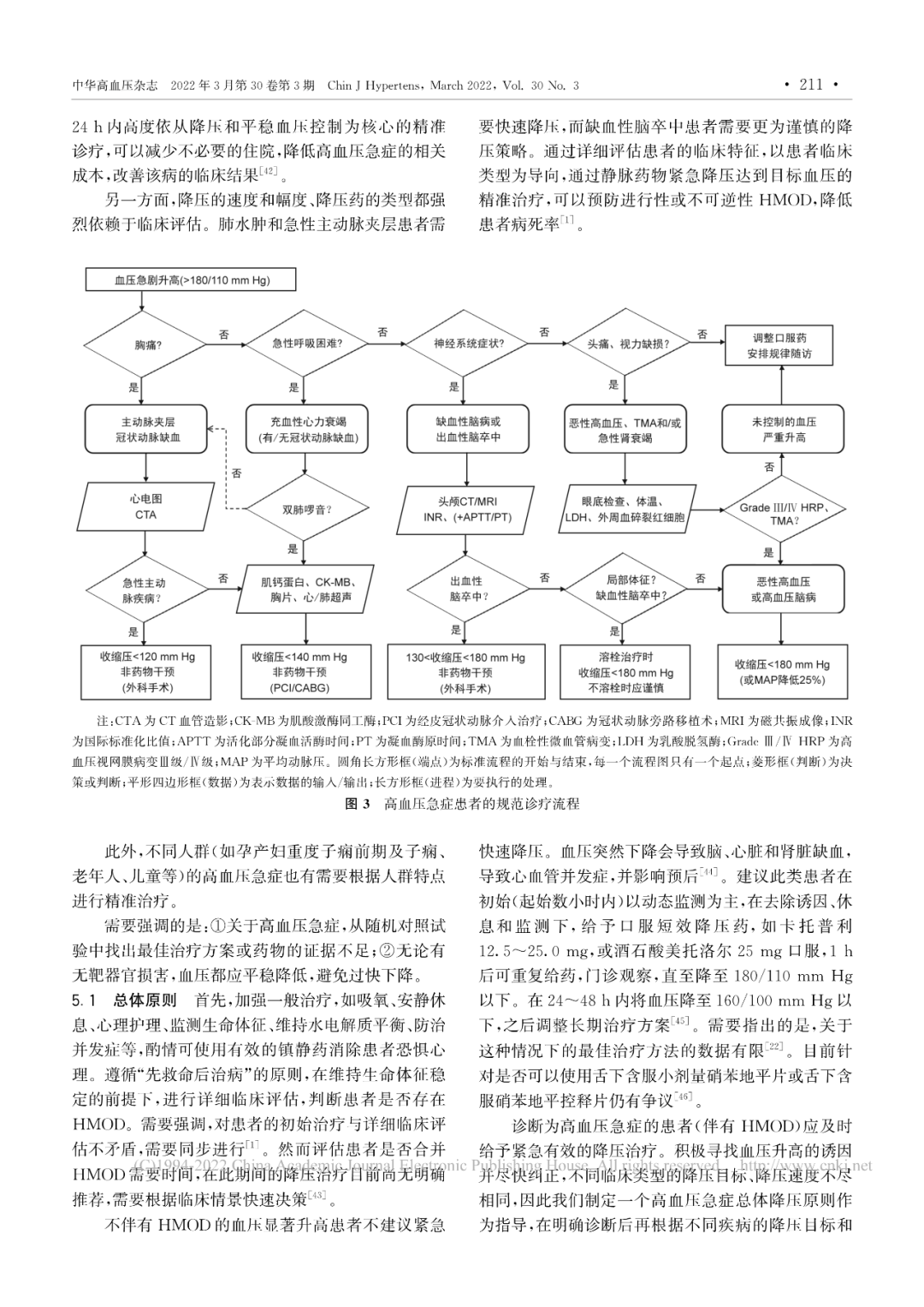
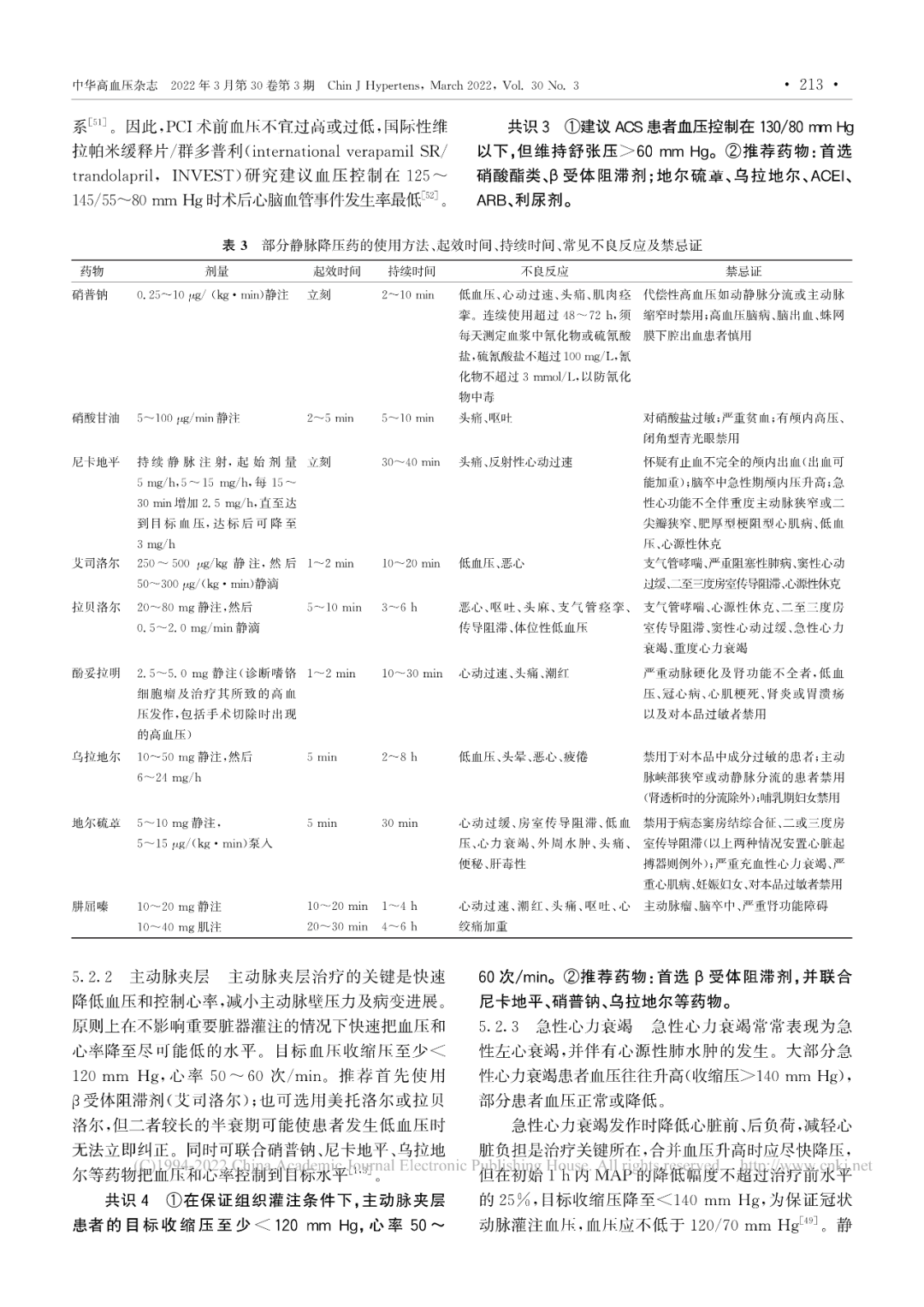
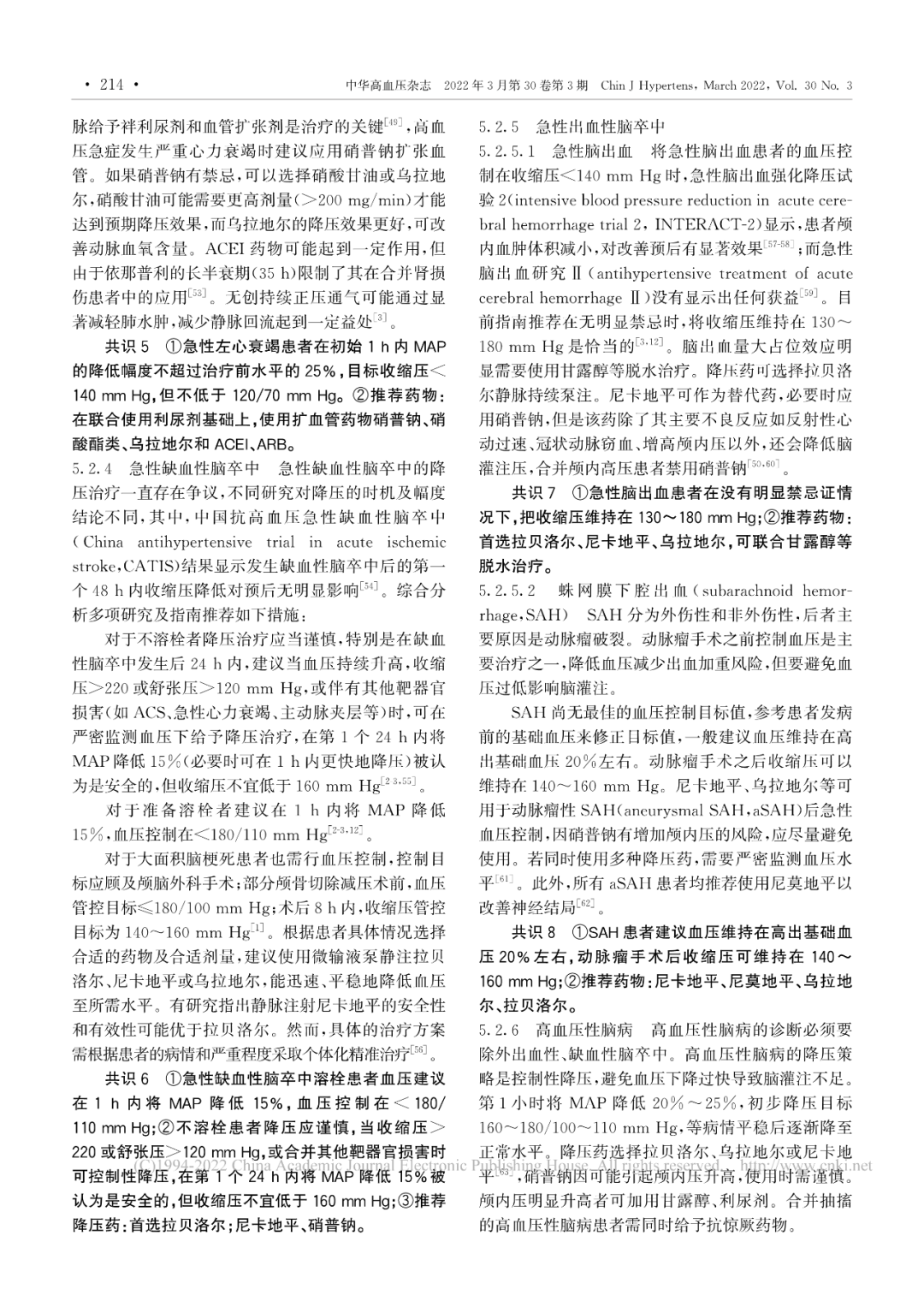
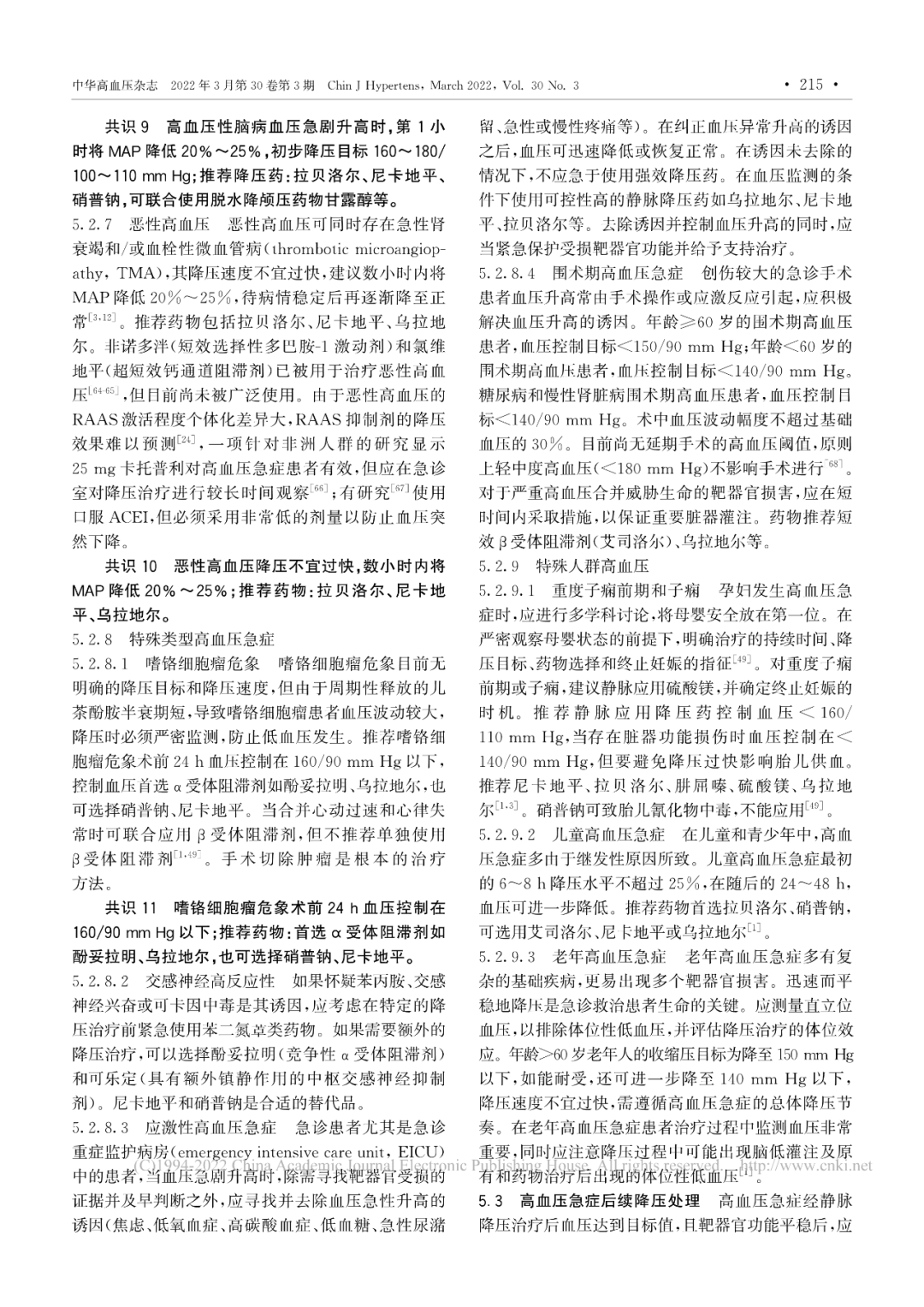
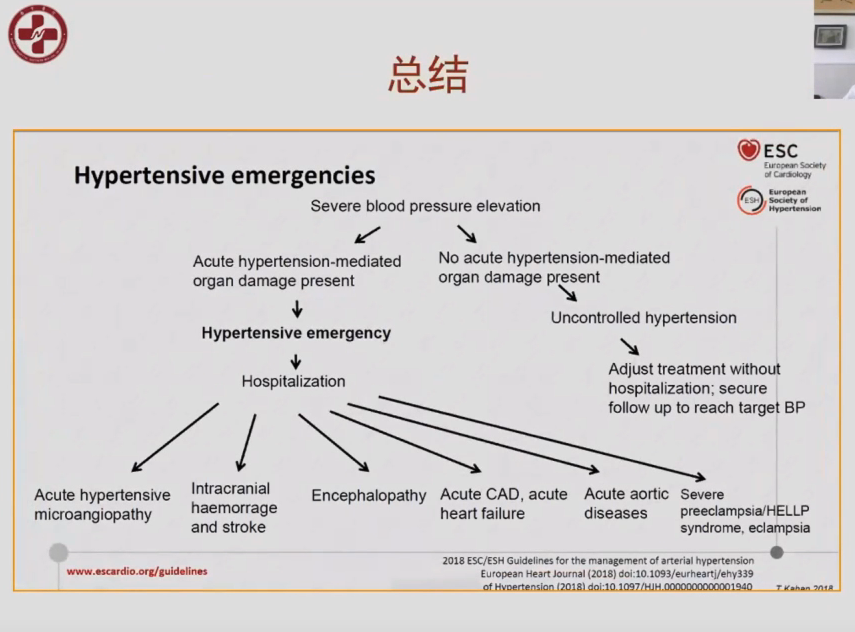
高血压急症是急诊科、心血管科及很多临床科室经常面对的急危重症之一,起病急、预后转归变化大、病死率高是主要临床特点。为统一高血压急症的定义、诊断和治疗标准,规范临床诊治,改善患者预后及生活质量,中国医师

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#急症#
47
#专家共识#
63
#最新#
55
#中国专家共识#
47
#高血压急症#
48