南方医科大学南方医院 许顶立 教授
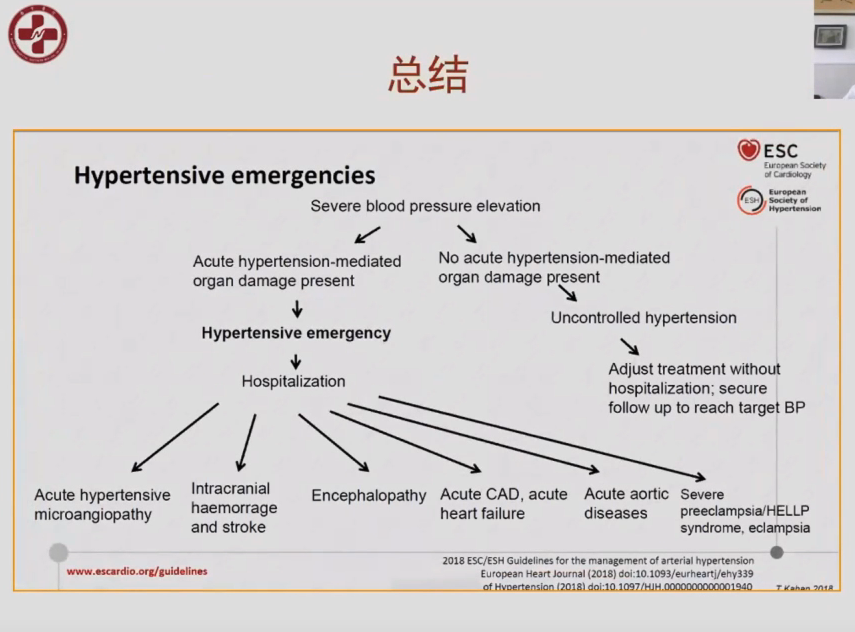
高血压急症是指在原发性或继发性高血压患者,在某些诱因作用下,血压突然和显著升高(一般超过180/120mmHg),同时伴有进行性心、脑、肾等重要靶器官功能急性损害的一种严重危及生命的临床综合征。高血压急症包括高血压脑病、颅内出血(脑出血和蛛网膜下腔出血)、脑梗死、急性心力衰竭、肺水肿、急性冠脉综合征、急性主动脉夹层、子痫等。在今年东方会OCC上,许顶立教授介绍高血压急症治疗中关键问题。
一部分高血压急症患者的血压值可能并不是特别高,如妊娠期或某些急进性肾小球肾炎的患者的高血压急症人群,但是,这些患者如果血压不及时控制在合理范围内,则会对脏器功能产生严重影响,甚至危及生命,处理过程中需要高度重视。而并发急性肺水肿、主动脉夹层、心肌梗死的患者,即使血压仅为中度升高,也应视为高血压急症。这非常值得临床重视。
临床上,高血压急症要注意与高血压亚急症相鉴别,后者是指血压明显升高但不伴靶器官损害。血压升高的程度不是区别二者的标准,区别的唯一标准是有无新进发生的急性进行性的严重靶器官损害。许多高血压亚急症患者可以通过口服降压药控制,初始治疗可以在门诊或急诊室,用药后观察5~6小时。2~3天后门诊调整剂量,具有高危因素的高血压亚急症如伴有心血管疾病的患者可以住院治疗。
当怀疑高血压急症时,应进行详尽的病史收集、体检和实验室检查,评价靶器官功能受累情况,以尽快明确是否为高血压急症。但初始治疗不要因为对患者整体评价过程而延迟。高血压急症的患者应进入急诊抢救室或加强监护室,持续监测血压。尽快应用合适的降压药;酌情使用有效的镇静药以消除患者恐惧心理。同时应针对患者不同的靶器官损害给予相应的处理。
·在严密监测血压、尿量和生命体征的情况下,应视临床情况的不同使用短效静脉降压药物;
·降压过程中严密观察靶器官功能状况,如神经系统症状和体征的变化,胸痛是否加重等;
·由于已经存在靶器官损害,过快或过度降压可能导致组织灌注压降低,诱发缺血事件。因起始的降压目标并非使血压正常,而是渐进地将血压调控至不太高的水平,最大限度地防止或减轻心、脑、肾等靶器官损害;
·在处理高血压急症时,应注意针对已经出现的靶器官损害进行治疗。
·一般情况下,初始阶段(数分钟到1小时内)血压控制的目标为平均动脉压的降低幅度不超过治疗前水平的25%;
·在随后的2~6小时内将血压降至较安全水平,一般为160/100 mmHg左右,如果可耐受这样的血压水平,临床情况稳定,在以后24~48小时逐步降低血压达到正常水平;
·降压时需要充分考虑到患者的年龄、病程、血压升高的程度、靶器官损害和合并的临床状况,因人而异地制定具体的方案;
·一旦达到初始靶目标血压,可以开始口服药物,静脉用药逐渐减量至停用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#急症#
42
#许顶立#
48
#OCC#
44
#OCC 2020#
40
#高血压急症#
40