Acta Biomater:具有免疫调节功能的组织工程支架可促进血管生成
2018-04-03 MedSci MedSci原创
为了促进组织工程骨的血管化,将IFN-γ极化巨噬细胞至M1加载到5%硅酸钙/β-磷酸三钙(CaSiO3-β-TCP)支架上。从支架释放的IFN-γ和Si分别使M1和M2巨噬细胞极化。 制备β-TCP、CaSiO3-β-TCP和IFN-γ@ CaSiO3-β-TCP,并评估其生物相容性。流式细胞术检测巨噬细胞的极化。培养人类脐静脉内皮细胞,并在从与负载巨噬细胞支架培养基中提取的诱导基质胶条件培养中诱
为了促进组织工程骨的血管化,将IFN-γ极化巨噬细胞至M1加载到5%硅酸钙/β-磷酸三钙(CaSiO3-β-TCP)支架上。从支架释放的IFN-γ和Si分别使M1和M2巨噬细胞极化。
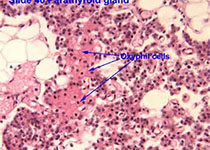
制备β-TCP、CaSiO3-β-TCP和IFN-γ@ CaSiO3-β-TCP,并评估其生物相容性。流式细胞术检测巨噬细胞的极化。培养人类脐静脉内皮细胞,并在从与负载巨噬细胞支架培养基中提取的诱导基质胶条件培养中诱导以评估血管生成。将支架皮下植入C57B1/6四周后,通过肉眼观察,苏木精和伊红染色以及CD31的免疫组织化学评估血管形成。
结果表明,IFN-γ@CaSiO3-β-TCP支架在早期(1-3天)释放IFN-γ,刺激巨噬细胞M1分化,然后释放Si诱导的巨噬细胞至M2极化,同时降解支架。M1/M2的激活使巨噬细胞分泌更多细胞因子,包括VEGF、CXCL12和PDGF-BB。与对照组相比,IFN-γCaSiO3-β-TCP支架在体外和体内形成更多的血管。
该研究表明,利用宿主巨噬细胞的具有免疫调节功能的组织工程支架可增加组织工程骨的血管化,为加速组织工程支架的血管化和骨生成提供了新的策略,并显示出治疗临界骨缺损的潜力。
原始出处:
Li T, Peng M, et al., 3D-printed IFN-γ-loading calcium silicate-β-tricalcium phosphate scaffold sequentially activates M1 and M2 polarization of macrophages to promote vascularization of tissue engineering bone. Acta Biomater. 2018 Mar 14. pii: S1742-7061(18)30132-6. doi: 10.1016/j.actbio.2018.03.012.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Bio#
30
#CTA#
26
#组织工程#
23
红红火火恍恍惚惚哈哈哈哈
55
不错
63