Biomed Res Int:疾病的检测,外泌体或许比血浆更合适
2017-08-07 MedSci MedSci原创
MicroRNAs(miRNAs)是小的非编码RNA,参与调节了许多生物过程。既往研究表明人血浆中富含miRNA,血浆来源的外泌体可作为新的诊断标志物。本研究旨在确定血浆及血浆外泌体中miRNA的表达水平差异。研究人员采集了健康人群的血浆及血浆来源的外泌体,进行测序和定量分析,然后使用qRT-PCR在两组肺癌样本中验证其中3个miRNAs。结果显示,血浆与外泌体内仅有几个miRNAs的表达存在差异
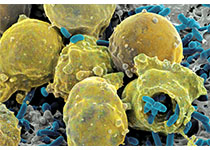
MicroRNAs(miRNAs)是小的非编码RNA,参与调节了许多生物过程。既往研究表明人血浆中富含miRNA,血浆来源的外泌体可作为新的诊断标志物。本研究旨在确定血浆及血浆外泌体中miRNA的表达水平差异。
研究人员采集了健康人群的血浆及血浆来源的外泌体,进行测序和定量分析,然后使用qRT-PCR在两组肺癌样本中验证其中3个miRNAs。
结果显示,血浆与外泌体内仅有几个miRNAs的表达存在差异,而qRT-PCR进一步验证了大部分miRNAs并不存在一致性差异。然而,在肺癌样本中两种上调的miRNA(miR-181b-5P和miR–21-5P)在外泌体内的水平显著高于血浆中的水平。
该研究首次对比了健康人群中血浆miRNA与外泌体miRNA的差异。结果表明,二者的miRNA的水平相似,但是在肺癌患者中两种肿瘤相关的miRNA在外泌体中的水平显著高于血浆水平。
原始出处:
Fei Tian, Yanting Shen, et al., No Significant Difference between Plasma miRNAs and Plasma-Derived Exosomal miRNAs from Healthy People. Biomed Res Int. 2017; 2017: 1304816. Published online 2017 Jun 1. doi: 10.1155/2017/1304816.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Bio#
34
#Med#
46
学习了,谢谢分享
89
不错的文章值得学习
76
好好文章学习了
75