JAMA子刊:创伤患者置入下腔静脉滤器,不能改善死亡率
2016-10-12 MedSci MedSci原创
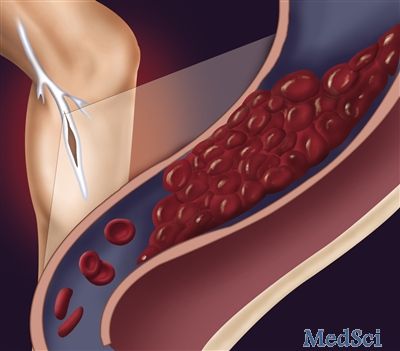
因外伤入院的患者其出血和血栓形成风险均增加。这类患者中下腔静脉滤器(IVC)的使用一直在增加,但缺乏高质量的证据证明其疗效。这项回顾性队列研究采用分层3:1倾向匹配法,选择相似的患者安置下腔静脉滤器,多变量逻辑回归模型根据年龄、性别、种族/民族、损伤严重度评分等来计算倾向评分。根据受伤日期进行分层匹配。使用多变量逻辑回归分析比较两组住院死亡率,调整年龄、性别、种族/种族、损伤严重程度评分、头部和颈
因外伤入院的患者其出血和血栓形成风险均增加。这类患者中下腔静脉滤器(IVC)的使用一直在增加,但缺乏高质量的证据证明其疗效。
这项回顾性队列研究采用分层3:1倾向匹配法,选择相似的患者安置下腔静脉滤器,多变量逻辑回归模型根据年龄、性别、种族/民族、损伤严重度评分等来计算倾向评分。根据受伤日期进行分层匹配。
使用多变量逻辑回归分析比较两组住院死亡率,调整年龄、性别、种族/种族、损伤严重程度评分、头部和颈部简短损伤评分的脑损伤程度。对所有患者损伤后24小时、48小时和72小时,还有出院时数据进行分析,确定死亡率的显著差异。
451例使用下腔静脉滤器的创伤患者和1343例匹配的无下腔静脉滤器的对照组,平均(SD)年龄为47.4(21.5)岁。总体的平均损伤严重度评分为24(范围1-75)。
平均随访3.8年(范围,0-9.4年),损伤后存活超过24小时的人群中,试验组和对照组的总死亡率或死亡原因没有差异,独立于置入下腔静脉滤器时存在或不存在深静脉血栓形成或肺栓塞。出院后6个月和1年的干预进行额外分析,没有发现两组患者间死亡率和死因的差异。8%(38/451)的患者在随访期间取出了下腔静脉过滤器。
本文的研究表明,创伤患者无论是否存在静脉血栓,置入或不置入下腔静脉滤器,对生存无显著差异。在这一人群中使用下腔静脉过滤器应重新审视,因为过滤器的取出率很低,一直留在人体内,会增加患者发病风险。
原始出处:
Shayna Sarosiek, MD1; Denis Rybin, PhD2; Janice Weinberg, ScD3; et al.Association Between Inferior Vena Cava Filter Insertion in Trauma Patients and In-Hospital and Overall Mortality. JAMA Surg. Published online September 28, 2016. doi:10.1001/jamasurg.2016.3091
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#静脉#
35
#下腔静脉#
43
#腔静脉滤器#
44
谢谢学习谢谢
53
#创伤#
37