Cell:协和医学院李平平教授等揭示二型糖尿病逆转新希望
2016-11-07 佚名 药明康德
最近,中国医学研究院北京协和医学院的李平平教授和美国加州大学圣地亚哥分校Jerrold M. Olefsky教授的联合团队在糖尿病及肥胖症研究领域取得重要发现,揭示了通过阻断galectin-3 (Gal3)这一蛋白,可以有效逆转糖尿病或肥胖症模型小鼠的胰岛素抵抗和葡萄糖不耐受等症状。这一成果发表于近期的《Cell》期刊上。▲李平平教授(左)和Jerrold M. Olefsky教授(右)(图片来
最近,中国医学研究院北京协和医学院的李平平教授和美国加州大学圣地亚哥分校Jerrold M. Olefsky教授的联合团队在糖尿病及肥胖症研究领域取得重要发现,揭示了通过阻断galectin-3 (Gal3)这一蛋白,可以有效逆转糖尿病或肥胖症模型小鼠的胰岛素抵抗和葡萄糖不耐受等症状。这一成果发表于近期的《Cell》期刊上。

▲李平平教授(左)和Jerrold M. Olefsky教授(右)(图片来源:北京协和医学院和UCSD官网)
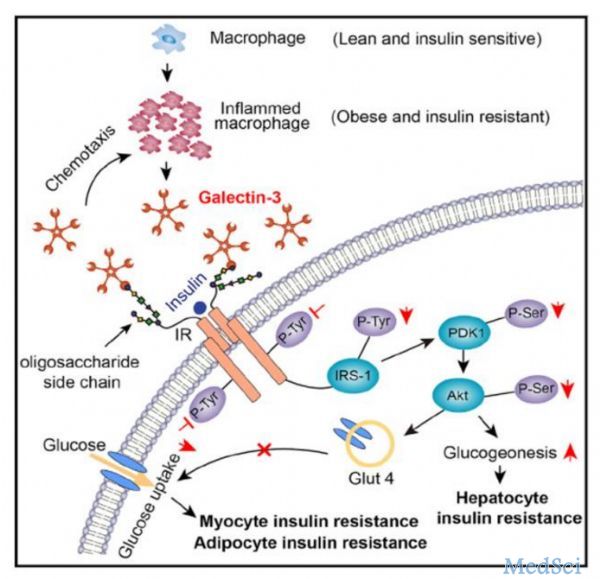
可由肥胖症引起的胰岛素抵抗(体细胞对胰岛素反应性的减弱)是二型糖尿病的一个主要症状。该症状的发生可能与巨噬细胞有关。在肥胖症个体中,巨噬细胞等免疫细胞富集于胰岛素目标部位(如肝脏、肌肉、脂肪组织等),会大量分泌TNFα和IL1β等炎症因子,后者可能会因干扰胰岛素下游信号通路而造成胰岛素抵抗。然而,之前的研究显示,通过阻断上述炎症因子并不能有效缓解胰岛素抵抗。因此,这里一定有着其他的机制在发挥作用。
李平平和Jerrold M. Olefsky教授的团队发现,问题的关键很可能就在于Gal3。它是一种凝集素糖蛋白,主要由巨噬细胞分泌,在患有肥胖症的人体和小鼠血液中水平偏高。巨噬细胞分泌的Gal3具有趋化效应,会吸引更多的巨噬细胞前来聚集,从而引起正反馈循环,导致出现持续性的炎症反应。
▲Gal3引发胰岛素抵抗机制(图片来源:Cell)
研究者们还发现,Gal3还可直接结合细胞表面的胰岛素受体,Gal3可阻止其与胰岛素的结合,抑制胰岛素受体下游的信号通路,从而导致出现胰岛素抵抗。如果将GAL3基因敲除或者用抑制剂(compound 47)阻断Gal3,上述小鼠中的胰岛素抵抗和葡萄糖不耐受等症状则可被逆转,恢复到正常水平。不过,肥胖这一表型并不会因此改变。在体外实验中,Gal3可抑制肌细胞和脂肪细胞在胰岛素刺激下对葡萄糖的摄取,并降低胰岛素对小鼠肝细胞分泌葡萄糖的抑制作用。
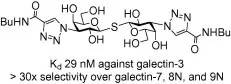
▲Compound 47结构(图片来源:Bioorganic & Medicinal Chemistry)
“这一研究在小鼠模型中将Gal3与胰岛素抵抗和葡萄糖不耐受联系起来,”Jerrold M. Olefsky教授说道:“它提示了,对Gal3的抑制可能是一种有效的糖尿病疗法。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
25
#新希望#
26
#Cell#
26
#医学院#
25
#二型糖尿病#
31
讲得好学习了
65
#协和医学院#
33
#协和#
30