J Bone Oncol:接受激素剥夺治疗的癌症患者脊柱骨折的预测:骨折风险评估工具(FRAX)和骨密度在现实生活临床实践中的可靠性
2022-09-05 医路坦克 MedSci原创
目前的指南建议使用骨矿物质密度(BMD)和世卫组织骨折风险评估工具(FRAX)来识别骨折风险较高的癌症患者,本文中我们研究了FRAX算法和骨密度在鉴别HDTs期间发生椎体骨折的乳腺癌和前列腺癌
骨骼脆性是早期乳腺癌女性和非转移性前列腺癌男性的一个重要临床问题。癌症治疗,如绝经前妇女的促性腺激素释放激素激动剂(GnRHa)和化疗诱导的卵巢衰竭,绝经后妇女的芳香酶抑制剂(AIs ),以及非转移性前列腺癌男性的抗雄激素治疗,会导致骨质流失,并伴有脆性骨折的高风险
接受激素剥夺疗法(HDTs)的受试者中有相当数量的人会发生脊椎骨折,尤其是在通过放射学和形态测量方法进行诊断时。然而,在这种临床情况下预测骨折是一个挑战,因为癌症治疗引起的骨丢失比原发性骨质疏松症更迅速和严重,并且在这种情况下骨折的决定因素仍然是未知的
目前的指南建议使用骨矿物质密度(BMD)和世卫组织骨折风险评估工具(FRAX)来识别骨折风险较高的癌症患者,以便在一级预防中使用骨活性药物进行治疗。这种方法通常用于治疗原发性骨质疏松症,但其在继发性骨质疏松症患者中的可靠性尚不清楚。此外,还不清楚患有前列腺癌的男性和患有乳腺癌的女性在暴露于HDTs时是否有不同的骨折风险
在这项研究中,我们研究了FRAX算法和骨密度在鉴别HDTs期间发生椎体骨折的乳腺癌和前列腺癌幸存者中的准确性。
设计:连续观察527例患者(女性乳腺癌429例,男性前列腺癌98例;中位年龄61岁),应用放射学和形态计量学方法对连续6个月以上的患者进行椎体骨折的评估,并分析其与FRAX评分、体重指数、骨密度、年龄和病程的关系。
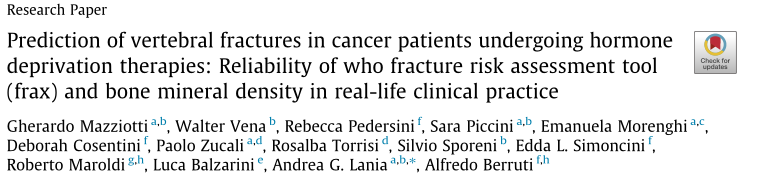
全脊椎骨折(VFs)的患病率,骨质疏松的密度诊断和主要骨折的FRAX评分?429例乳腺癌女性患者中有20例接受雌激素剥夺疗法,98例前列腺癌男性患者接受雄激素剥夺疗法。*,P < 0.001对男性;**,与女性相比,P < 0.001。P值来自卡方检验。
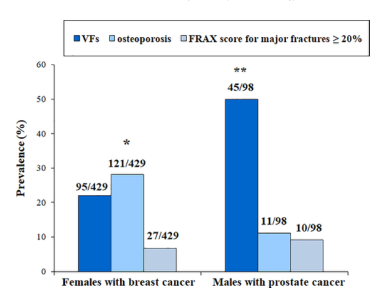
对527名受试者(429名女性乳腺癌患者和98名男性前列腺癌患者)进行激素剥夺治疗(HDTs)持续时间四分位数分层后,其椎骨骨折(VFs)的患病率。
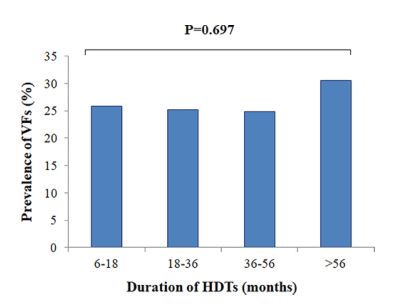
全脊椎骨折(VFs)和多发性/中度/重度VFs的患病率[即脊柱畸形指数(SDI)的患病率≥2]在98名接受雄激素剥夺治疗的前列腺癌男性中,根据体重指数(身体质量指数)进行分层。*,P < 0.001,而身体质量指数< 25千克/平方米。P值来自卡方检验。

接受雄激素剥夺治疗的前列腺癌男性(M)受试者亚组中椎体骨折(VFs)的风险,根据体重指数(身体质量指数)、骨密度(BMD)和阿比特龙治疗进行分层。当受试者和事件的数量允许进行统计分析时,报告每个根的优势比(OR)和95%置信区间。
结果:共发现脊柱骨折140例(26.6%),脊柱畸形指数与脊柱骨折持续时间显著相关(Rho0.38;p<0.001)。只有在女性中,椎体骨折与主要骨折的FRAX评分显著相关[OR1.08;P<0.001]。根据操作特征(ROC)分析计算的大型骨折FRAX评分的最佳分界值为6.35%。然而,在男性中,椎体骨折与体重指数±25 kg/m2(OR17.63;P<0.001)、任何骨骼部位骨密度T评分低于±1.0SD(OR7.79;P<0.001)以及促性腺激素释放激素激动剂(GnRHa)加阿比特龙治疗(OR11.51;P=0.001)显著相关。
结论:FRAX和BMD可用于预测接受HDTS治疗的受试者的椎体骨折,但其阈值似乎低于普通人群。高BMI是男性卧床时脊柱骨折的决定因素。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Bone#
49
#Oncol#
0
#评估工具#
46
#癌症患者#
49
#临床实践#
36
#骨折风险#
38