JAHA:癌症患者放射治疗与心血管疾病死亡之间的关联
2022-03-09 MedSci原创 MedSci原创
放疗与肺癌和支气管癌、子宫颈癌、子宫体癌和膀胱癌患者的心血管特异性生存率降低相关。放疗后应进行心血管状况的长期监测。
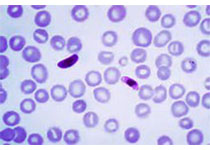
心血管疾病(CVD)和癌症是全球死亡的主要原因,它们之间有着复杂的关系。既往的研究表明,吸烟、酗酒、肥胖和不良的生活习惯是CVD和癌症的常见的可改变危险因素。癌症患者尤其是肺癌患者的心血管疾病发病率几乎是普通人群的两倍,这提供了癌症患者心血管死亡率较高的证据。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在调查癌症放疗与心血管疾病(CVD)死亡之间的关系,并评估普通人群和接受放疗的癌症患者中CVD死亡的相对风险。

研究人员从监测、流行病学和最终结局数据库中提取了16个地区的癌症统计数据并进行了评估。多变量Cox比例风险回归用于分析放疗与心血管特异性生存率之间的关联。通过比较观察到的接受放射治疗的癌症患者的死亡人数与一般人群的预期死亡人数来估计CVD死亡的标准化死亡率。

在从数据库中确定的2214944名患者中,292102人(13.19%)死于CVD。多变量Cox比例风险回归分析表明,放疗是肺癌和支气管癌、子宫颈癌、子宫体癌和膀胱癌患者心血管特异性生存的独立危险因素。接受放疗的癌症患者的长期心血管特异性生存率显著低于未接受放疗的患者。肺癌和支气管癌、子宫颈癌、子宫体癌和膀胱癌患者接受放射治疗的心血管疾病死亡发生率高于一般人群。标准化死亡率随着癌症诊断年龄的增加而显著降低,在诊断后10年内逐渐降低,而在诊断10年后逐渐增加。
由此可见,放疗与肺癌和支气管癌、子宫颈癌、子宫体癌和膀胱癌患者的心血管特异性生存率降低相关。放疗后应进行心血管状况的长期监测。
原始出处:
Enrui Liu.et al.Association Between Radiotherapy and Death From Cardiovascular Disease Among Patients With Cancer: A Large Population‐Based Cohort Study.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.023802.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
50
学习了,👍👍👍
52
#AHA#
43
#癌症患者#
51
#血管疾病#
46
学习学习
52
学习一下
64
学习了,谢谢分享
48