盘点:高尿酸血症近期重要研究进展汇总
2017-08-06 MedSci MedSci原创
我国高尿酸血症呈现高流行、年轻化、男性高于女性、沿海高于内地的趋势。据估算,全国人口的10%患高尿酸血症,而沿海和经济发达地区高尿酸血症的患病率甚至高达20%以上,我国高尿酸血症的患病率已经高于糖尿病的患病率。发病特点尤其以男性为主、特点“重男轻女”。由于患者无临床症状,往往不引起患者的注意,忽视了治疗。本文小编为大家整理汇总了近年来高尿酸血症相关研究进展,与大家分享。【1】我国汉族妇女血浆pro
我国高尿酸血症呈现高流行、年轻化、男性高于女性、沿海高于内地的趋势。据估算,全国人口的10%患高尿酸血症,而沿海和经济发达地区高尿酸血症的患病率甚至高达20%以上,我国高尿酸血症的患病率已经高于糖尿病的患病率。发病特点尤其以男性为主、特点“重男轻女”。由于患者无临床症状,往往不引起患者的注意,忽视了治疗。本文小编为大家整理汇总了近年来高尿酸血症相关研究进展,与大家分享。
【1】我国汉族妇女血浆proANP与高尿酸血症的关系
前心房尿钠肽(proANP)与高尿酸血症之间的关系在人群中尚未明确。近日,国际杂志 CCLM在线发表一项关于评估中国汉族妇女血浆proANP与高尿酸血症的关系的横断面研究。纳入了居住在苏州市姑苏区的1360名30岁以上女性。结果表明,中国汉族45岁以上老年人血浆proANP与高尿酸血症呈显著负相关趋势,增加血浆proANP应该是中老年妇女高尿酸血症的保护因素。
【2】协和研究称,我国高尿酸血症患病率为13%
北京协和医院学者开展的一项全国性研究表明,我国人群中高尿酸血症患病率为13%,男性中高达18.5%,明显高于女性(8.0%)。在65岁以下男性中,高尿酸血症患病率随年龄增长而降低,到65岁以上才又升高。而在≥35岁的女性中,高尿酸血症患病率随年龄增长一直升高。研究者认为,这可能与性激素的相互作用有关。就地域来说,南方地区和农村的高尿酸血症患病率高于北方地区和城市。按民族区分,回族中高尿酸血症患病率最低,男性中为8%,女性中仅3.8%。研究者还发现,高尿酸血症患者常合并多个心血管病危险因素。
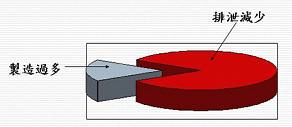
【3】高尿酸血症和尿酸过度排泄增加了2型糖尿病中单纯肾囊肿的风险
既往研究已经讨论了健康人中单纯肾囊肿(SRC)和血清尿酸水平之间的关系。新的一项横断面研究评估了2型糖尿病男性和绝经后女性血清尿酸水平与尿酸分泌排泄(FEUA)和单纯肾囊肿之间的关系。结果表明,高尿酸血症和高水平的FEUA是男性和绝经后2型糖尿病女性SRC发展的独立危险因素。一半过量产生高尿酸血症患者患有SRC。因此,高尿酸血症和/或高FEUA的2型糖尿病患者有SRC的风险。没有研究评估服用尿酸排泄剂的高尿酸血症或痛风患者的SRC患病率。需要进行前瞻性研究来探讨尿酸排泄物是否会影响SRC的发生。
【4】高尿酸血症对心血管疾病风险的预测情况
患者在不同状况下,高尿酸血症与患心血管疾病有关。新的一项研究测试了Cox模型中的尿酸(UA)是否能够使1522名初治高血压患者的心血管风险更好地分层,并保留患者肾功能。结果表明,UA是心血管结局的独立预测因子,并对心血管风险进行了重新分类。研究结果还表明,UA在具有正常肾功能的高血压患者中Cox模型的预后更加准确性。
【5】无症状高尿酸血症与 肾结石的发生独立相关
虽然痛风和肾结石之间的相关性已众所周知,但是无症状高尿酸血症和肾结石发生发展之间的关系很大程度上是未知的。近日,肾脏病领域权威杂志Am J Kidney Dis的一项研究纳入了239331名韩国成年人,随访1184653.8人年。结果表明,健康男性血尿酸水平升高与肾结石发生风险增加中度并且独立相关,而且以剂量依赖的方式。
【6】不伴合并症的无症状高尿酸血症可以预测心脏代谢性疾病
不伴合并症的无症状高尿酸血症是否会增加心脏代谢病和慢性肾脏病的风险仍存在争议。近日,心血管权威杂志Hypertension上发表了一篇研究明确了无症状高尿酸血症与心血管疾病间的相关性。该研究共纳入了5899例无合并症的患者,随访5年,结果发现高尿酸血症与高血压、血脂异常、慢性肾脏疾病和超重肥胖的累积发病率增加相关。表明,无症状高尿酸血症再无合并症的个体中发生心脏代谢疾病的风险显著。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研究进展#
51
#高尿酸#
50
学习一下谢谢分享
57
得到新知
65
知识积累,好东西值得拥有
73
得到新知
1
好东西
61
好东西学习了!
29
学习了,涨姿势
23
henhao
30