NEJM:血流储备分数指导的多支血管成形术在心肌梗死中的运用!
2017-03-19 xing.T MedSci原创
对于已经在梗死相关动脉进行PCI的STEMI和多支血管病变患者,在急性期FFR指导的非梗死相关动脉完全性血运重建会发生复合心血管终点风险,但低于在那些只处理梗死相关动脉患者的风险。
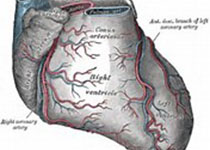
在ST段抬高心肌梗死(STEMI)患者中,进行经皮冠状动脉介入治疗(PCI)恢复梗死相关冠状动脉血流量可以改善预后。然而,PCI在非梗死相关冠状动脉中的应用仍存在争议。近日,顶级医学期刊NEJM上针对这一问题发表了一篇研究文章。研究人员将885例已经接受过PCI治疗梗死相关冠状动脉的STEMI和多支血管病变患者按1:2的比例进行随机化分组,分别接受进行血流储备分数(FFR)指导的非梗死相关冠状动脉PCI的完全血运重建(295例)或不进行非梗死相关冠状动脉血运重建(590例)。两组患者都进行了FFR检查,但在后一组中,病人和他们的医生都没有重视FFR的发现。主要终点为12个月内任何原因、非致死性心肌梗死、血运重建和脑血管事件的复合死亡。在完全血运重建组有23例患者发生研究主要终点事件,而在只在梗死动脉进行血运重建的不完全血运重建组患者有121例患者发生研究主要终点事件,即每100患者分别有8次和21次事件(风险比为0.35;95%可信区间为0.22-0.55;P<0.001)。在完全血运重建组有4例患者发生死亡,而不完全血运重建组有10例患者死亡(1.4% vs. 1.7%)(风险比为0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#成形术#
0
#多支血管#
34
#血管成形术#
36
学习了谢谢分享
62
文章很好,值得分享
0
路过。。。。。。。
47