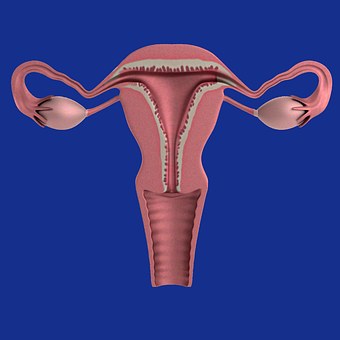
Obstet Gynecol:良性病变致子宫切除患者30天内再入院分析
2016-10-02 xing.T MedSci原创
由此可见,子宫切除术患者有出院后不久发生再入院的倾向,大多数再次入院是因为手术相关的问题,最常见的是手术部位感染。医疗并发症,包括静脉血栓栓塞,占再入院患者的比例少于10%。减少子宫切除患者再入院的工作重点应放在早期出院后的随访,预防感染等并发症。
近日,妇产科领域权威杂志《obstetrics and gynecology》发表了描述子宫良性疾病导致子宫切除术后30天内患者再住院相关的时间和原因分析文章。
研究者进行了一项回顾性分析,分析了从2012年到2013年美国外科医师学会的国家外科质量改进项目数据库收集的数据。研究者确定了所有良性子宫病变患者子宫切除术(通过开腹、腹腔镜、经阴道三种手术方式)后30天再入院情况。住院时间通过出院日期确定,并将入院诊断制成表格,统计分析包括χ2检验和多因素logistic回归分析。
研究者发现子宫切除患者30天内再入院率为2.8%(1118 / 40580例子宫切除术),开腹手术患者再入院为3.7%(361 / 9869)、腹腔镜手术患者再入院率为2.6%(576 / 22266),而阴道子宫切除术患者再入院率为2.1%(181 / 8445)。
由此可见,子宫切除术患者有出院后不久再入院的倾向,大多数再次入院是因为手术相关的问题,最常见的是手术部位感染。医疗并发症,包括静脉血栓栓塞,占再入院患者的比例少于10%。减少子宫切除患者再入院的工作重点应放在早期出院后的随访,预防感染等并发症。
原始出处:
Penn,Courtney A, et al. Timing of and Reasons for Unplanned 30-Day Readmission After
Hysterectomy for Benign Disease. obstetrics and gynecology.2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TET#
34
#NEC#
47
#30天#
45
文章真好,喜欢阅读
55
好文章,长见识
55
#子宫切除#
44