Cerebrovasc Dis:脑出血中的淀粉样血管病
2018-04-18 国际循环编辑部 国际循环
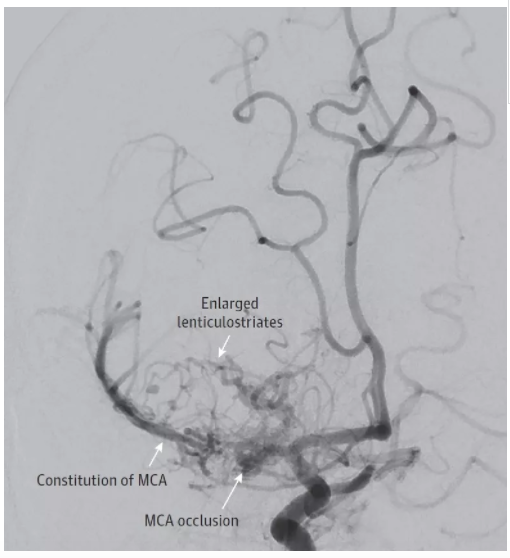
脑出血(ICH)的危险因素包括高血压和脑淀粉样血管病(CAA)。近日,巴黎狄德罗大学Guidoux C等发表于Cerebrovascular Diseases杂志的一项研究旨在探讨确定ICH死亡患者中CAA发病率,CAA与其他危险因素的可能潜在重叠因素,以及CAA与脑微出血灶的相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
38
#Dis#
23
#血管病#
32
好文献.学习了
47
学习一下谢谢
55
^_^^_^^_^^_^
52
谢谢分享学习了
44