JNS:内镜治疗高血压脑出血
2018-03-26 杨中华 脑血管病及重症文献导读
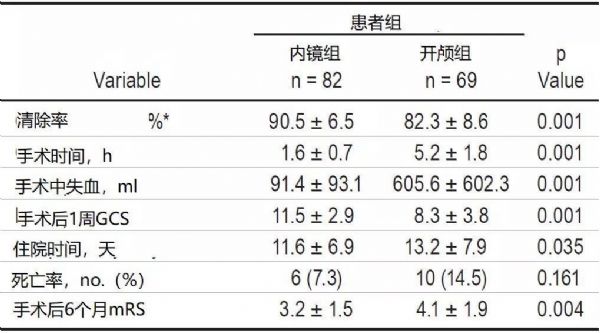
自发性脑出血占所有卒中的10-30%,是卒中相关死亡和致残的主要原因。高血压脑出血是最常见的脑出血类型,三十天死亡率高达40%,幸存者往往也遗留严重残疾,给家庭和社会带来极大的负担。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内镜#
0
#内镜治疗#
38
学习了
54
学习
69
很先进的技术.学习了
58
好.学习.
54
学了
60
学了
28