慢性血栓栓塞性肺动脉高压患者在一系列球囊肺血管成形术后肺动脉重塑阳性
2022-08-31 刘少飞 MedSci原创
证明慢性血栓栓塞性肺动脉高压(CTEPH)患者在球囊肺血管成形术(BPA)后肺动脉重塑的积极性。
研究目的:
证明慢性血栓栓塞性肺动脉高压(CTEPH)患者在球囊肺血管成形术(BPA)后肺动脉重塑的积极性。
设计和方法:
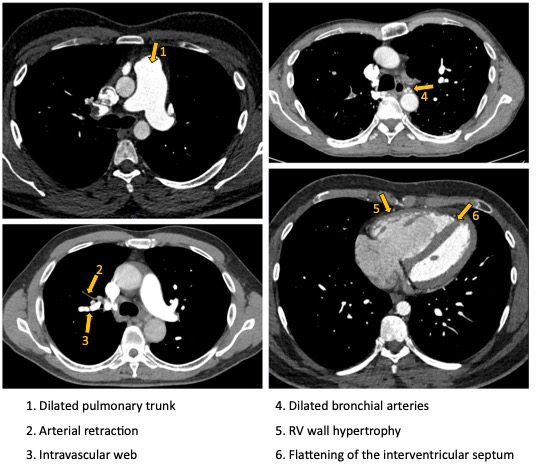
一位68岁的女性因脚和腿肿胀,动脉血饱和度低(92%)而被送入肺动脉高压科。她通过两次肺栓塞发作--住院前7年和5年。患者接受了抗凝剂(华法林)、利尿剂(呋塞米、螺内酯)治疗。有创肺血管造影证实了肺动脉的血栓栓塞性病变。除CTEPH外,其他类型的肺动脉高压均被排除。多学科委员会认为她因肥胖和不明原因的贫血而无法手术。但在技术上有可能进行BPA。该患者接受了5次BPA治疗。在第一次BPA之前和之后以及最后一次BPA之后3个月,进行了肺动脉血管内超声(IVUS)检查。
研究结果:
根据治疗结果,患者的功能等级有所提高(从4级到3级),6分钟步行测试的距离略有增加(从290米到303米),肺动脉的平均预压力从40毫米汞柱下降到35毫米汞柱。在评估肺动脉的大小时,进行了血管成形术,确定有积极重塑的迹象(表1)。根据侵入性血管造影,节下动脉的分支直径增加了14.3%。根据IVUS的结果,得到了类似的结果。管腔直径增加了10%。
研究结论:
CTEPH患者成功的BPA系列可以导致肺动脉的显著正向重塑。
参考文献:
Yarovoy S, Chazova I, Danilov N, Matchin Y. POSITIVE PULMONARY ARTERY REMODELING AFTER A SERIES OF BALLOON PULMONARY ANGIOPLASTIES IN A PATIENT WITH CHRONIC THROMBOEMBOLIC PULMONARY HYPERTENSION. J Hypertens. 2022 Jun 1;40(Suppl 1):e264. doi: 10.1097/01.hjh.0000838224.40623.76. PMID: 36027325.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#成形术#
41
#动脉高压#
49
#血管成形术#
51
#肺动脉高压患者#
55
#球囊#
0
#球囊肺血管成形术#
45