BMPR2点突变转基因大鼠加重实验性肺动脉高压
2022-04-14 刘少飞 MedSci原创
携带 2 型骨形态发生蛋白受体 ( Bmpr2 ) 突变的肺动脉高压 (PAH) 患者出现严重血流动力学损害的时间较早,并且与没有突变的患者相比,生存结果较差。
肺动脉高压(PAH)是一种严重的渐进性疾病,其特点是闭塞性肺血管病(PVD)导致的肺血管阻力增加,导致右心衰竭,最终导致死亡。由于70%的遗传性PAH和15-40%的明显散发性PAH是在单倍体骨形态发生蛋白2型受体(Bmpr2)突变的基础上发展起来的,所以Bmpr2被认为是发展PAH的主要遗传风险因素。在临床上,有Bmpr2突变的PAH患者已被证明发病早、预后差、血管反应性降低、右心室功能受损、对PAH特异性治疗有抵抗力。在实验中,Bmpr2的单倍体功能不足通过阻碍肺内皮细胞和平滑肌细胞的功能,包括凋亡、增殖、分化和炎症以及右心室功能,牵涉到PVD和PAH病理的发展。在肺动脉高压(PH)的模型中,Bmpr2的作用也被广泛研究,使用了转基因小鼠。然而,由于在小鼠模型中很难再现人类PAH的进行性特征,因此很难评估Bmpr2在进行性PVD发展中的作用及其与生存的相关性。因此,Bmpr2突变在临床表型中的作用,特别是突变携带者和非携带者之间的生存差异及其与PVD发展的关系,在实验性PH模型中很少被探讨。
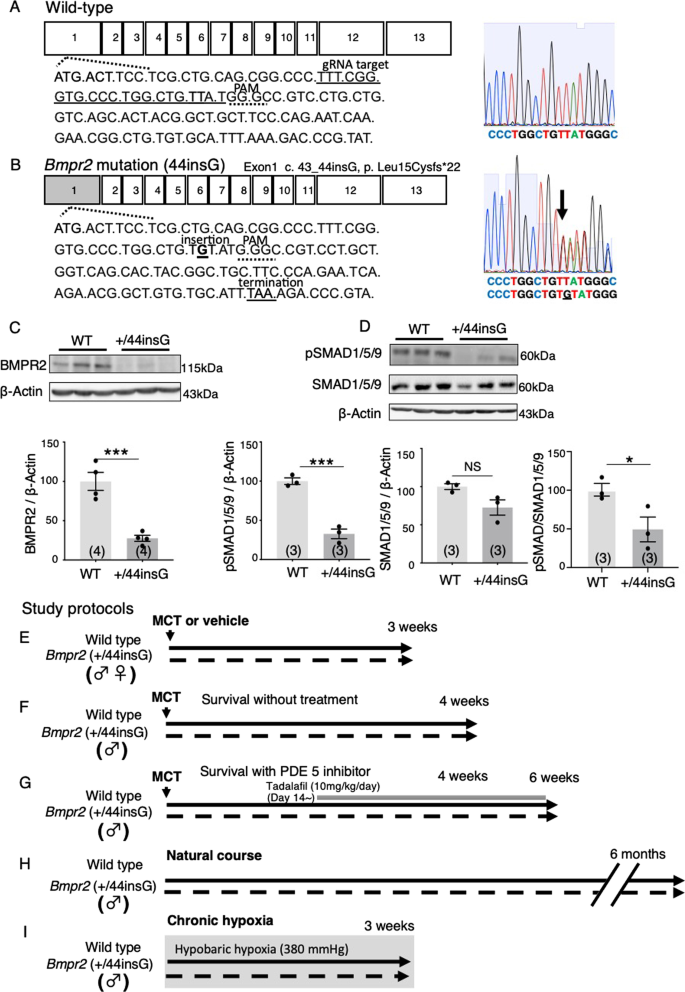
在本研究中,我们建立了一个大鼠模型,利用CRISPR/Cas9基因组编辑方法,在Bmpr2中引入了一个单核苷酸插入,并测试了单倍体Bmpr2突变是否影响MCT诱导的大鼠进行性PH。
研究方法:
利用CRISPR/Cas9在大鼠体内产生了Bmpr2第1外显子的单等位单核苷酸插入(+/44insG),然后评估了PH、肺血管疾病(PVD)和注射MCT后的生存率,是否有5型磷酸二酯酶抑制剂他达拉非的作用。
研究结果:
与野生型相比,+/44insG大鼠在肺部的BMPR2信号减少。
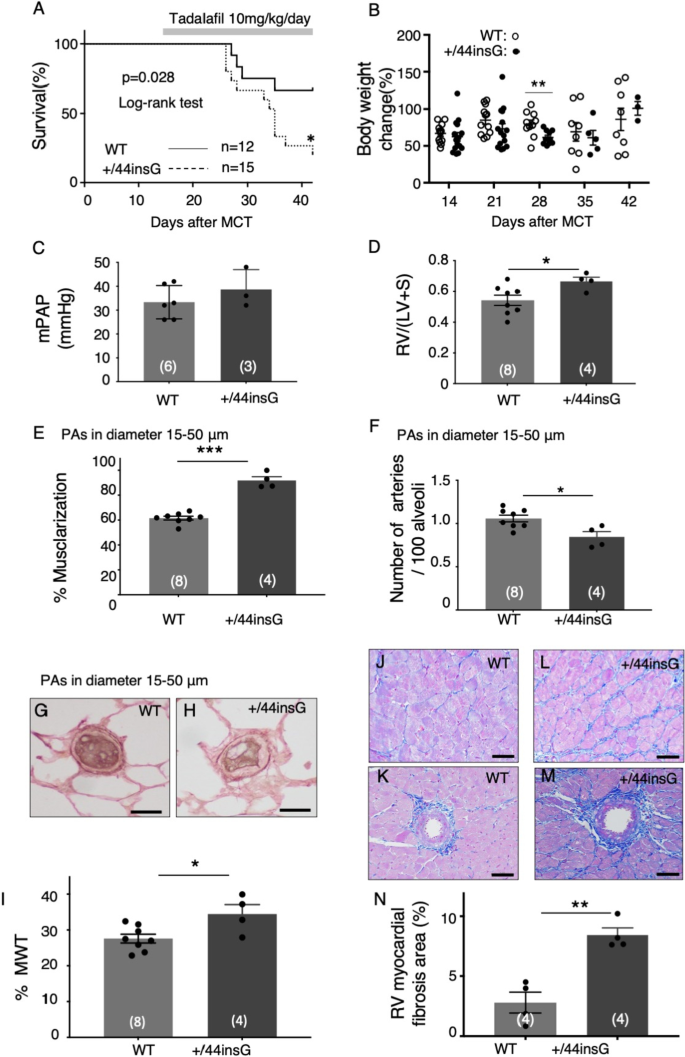
注射MCT后3周评估的PH值和PVD值在野生型和+/44insG大鼠中相似。
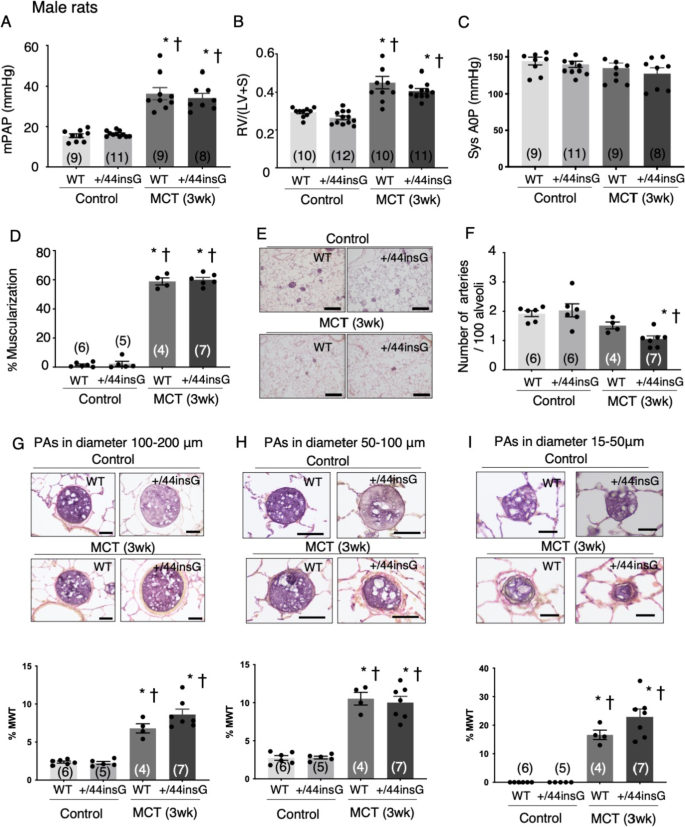
然而,注射MCT后4周的存活率在+/44insG大鼠中明显降低。在注射MCT后4周存活的大鼠中,+/44insG大鼠的右心室与左心室及室间隔的重量比(RV/[LV+S])和肺动脉(PAs)的内侧壁厚度(MWT)百分比增加。
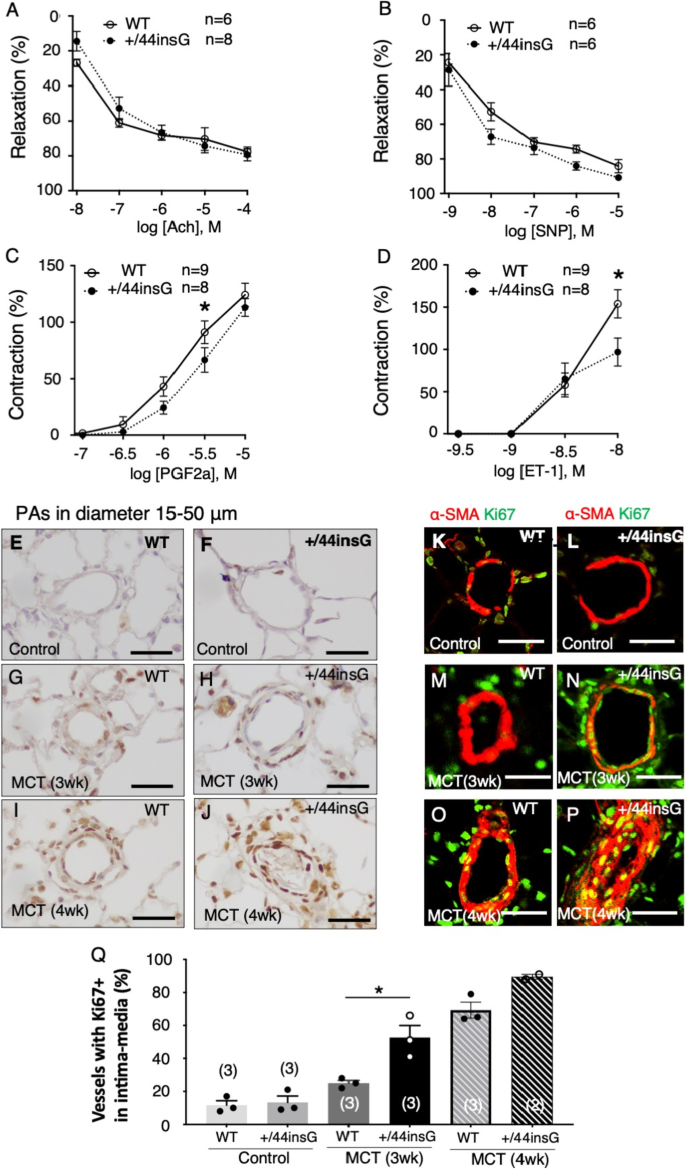
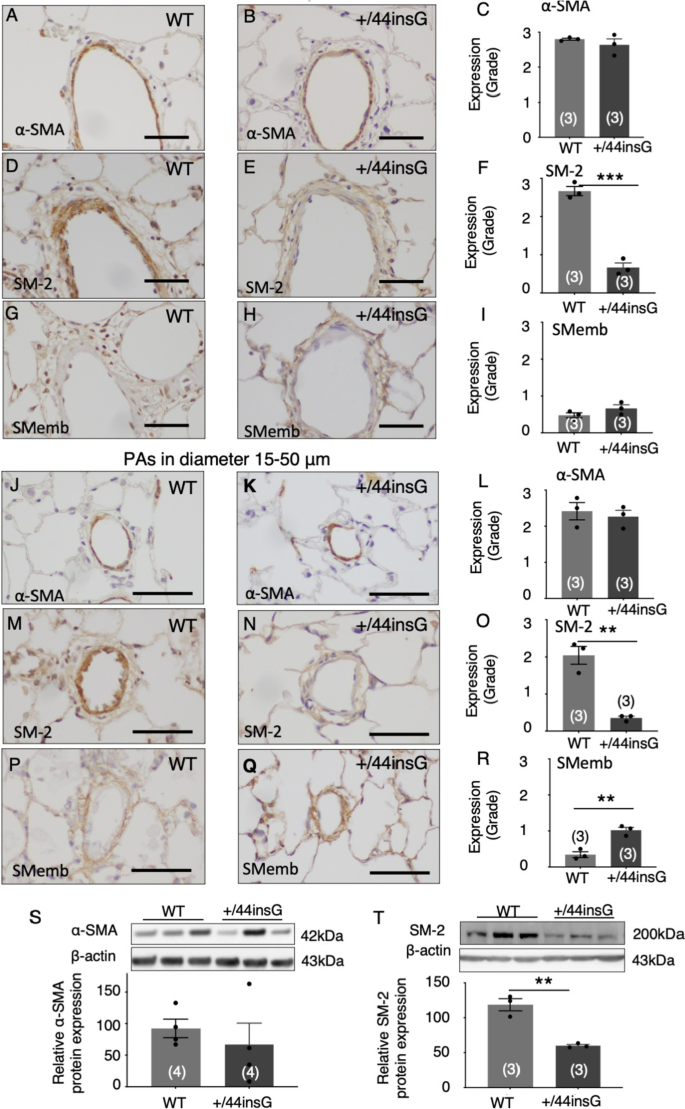
免疫组化分析显示,与野生型相比,在注射MCT后3周,+/44insG大鼠肺部Ki67阳性细胞的血管增加,PAs中成熟和未成熟的平滑肌细胞表型标志物减少。
对前列腺素-F2α和内皮素-1反应的PA收缩在+/44insG大鼠中明显减少。与野生型相比,接受过他达拉非的+/44insG大鼠生存状况更差,RV/(LV+S)、远端PA的%MWT和RV心肌纤维化显著增加。
研究结论:
本研究表明,Bmpr2突变可促进PA平滑肌细胞的去分化、晚期PVD和RV心肌纤维化,并对大鼠MCT-PH的自然和治疗后过程产生不利影响,仅在晚期阶段有明显影响,因此需要利用这种新的遗传模型进行临床前研究,以优化遗传性PAH的治疗效果。
参考文献:
Kabwe JC, Sawada H, Mitani Y, Oshita H, Tsuboya N, Zhang E, Maruyama J, Miyasaka Y, Ko H, Oya K, Ito H, Yodoya N, Otsuki S, Ohashi H, Okamoto R, Dohi K, Nishimura Y, Mashimo T, Hirayama M, Maruyama K. CRISPR-mediated Bmpr2 point mutation exacerbates late pulmonary vasculopathy and reduces survival in rats with experimental pulmonary hypertension. Respir Res. 2022 Apr 8;23(1):87. DOI: 10.1186/s12931-022-02005-w. PMID: 35395852.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#动脉高压#
40
#BMP#
46
#实验性#
43
精彩评论,需要您登录查看
58
#转基因#
59