Cancer Cell:曹雪涛团队发现肿瘤相关巨噬细胞促进肿瘤转移和化疗抵抗的新机制
2022-09-11 中国医学科学院新闻中心 中国医学科学院新闻中心
在肿瘤微环境中存在的多种免疫细胞受到肿瘤细胞及其微环境中信号、营养物质介导的驯化并参与肿瘤的免疫逃逸和助力肿瘤细胞的生长和转移。
2022年9月8日,中国医学科学院基础医学研究所暨中国医学科学院免疫治疗研究中心曹雪涛院士团队在Cancer Cell在线发表了题为“Increased glucose metabolism in TAMs fuels O-GlcNAcylation of lysosomal Cathepsin B to promote cancer metastasis and chemoresistance”的研究论文。该研究报道了肿瘤相关巨噬细胞(tumor associated macrophage,TAM)中葡糖糖代谢通过增强溶酶体组织蛋白酶——Cathepsin B的O连接的N乙酰葡糖胺糖基化修饰( O-linked N-acetylglucosamine,O-GlcNAcylation)促进了肿瘤转移和化疗抵抗,首次揭示了M2样TAM是肿瘤微环境中葡萄糖摄取能力最强的免疫细胞亚群,首次发现了定位于溶酶体的O-连接的N-乙酰葡萄糖胺转移酶(O-Linked N-Acetylglucosamine Transferase,OGT)的新功能(见图1)。
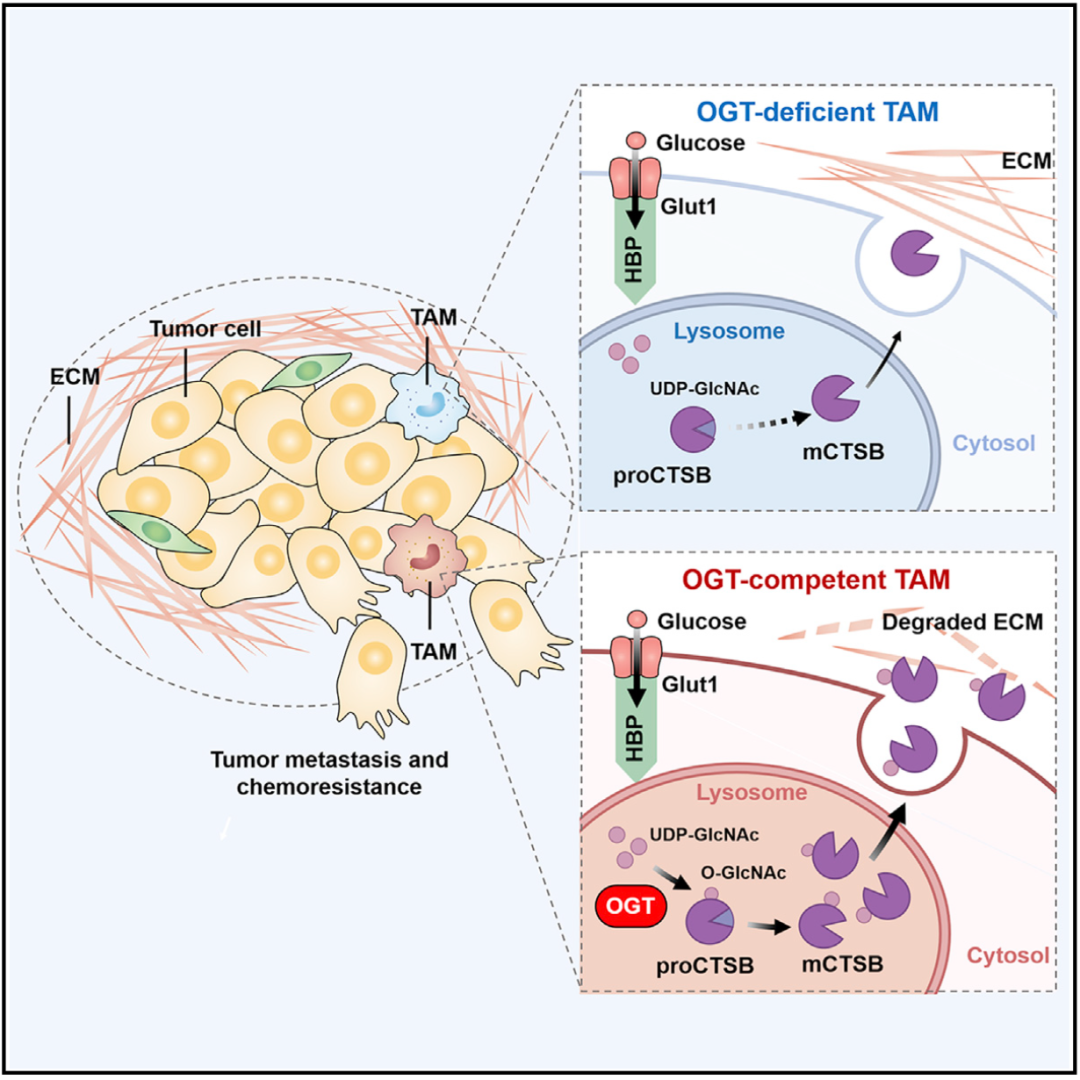
图1.TAM通过葡萄糖代谢和O-GlcNAcylation修饰促进肿瘤的转移和化疗抵抗
在肿瘤微环境中存在的多种免疫细胞受到肿瘤细胞及其微环境中信号、营养物质介导的驯化并参与肿瘤的免疫逃逸和助力肿瘤细胞的生长和转移。TAM作为一种主要的肿瘤浸润免疫细胞,M1样TAM可能参与抑制肿瘤进展,而M2样TAM能够促进肿瘤的生长、侵袭、血管生成以及化疗抵抗。对于TAM及其亚型的葡萄糖吸收及其胞内代谢如何塑造M2样TAM特异性功能,以促进肿瘤的转移和化疗抵抗是肿瘤免疫学领域亟待探究的一个重要科学问题。
该研究的主要发现及创新点包括:一是在TME中,与M1样TAM及其他免疫细胞相比,M2样TAM具有更强的单细胞葡萄糖吸收能力;二是TAM吸收的葡萄糖通过氨基己糖生物合成途途径(HBP)促进溶酶体OGT对Cathepsin B Ser210进行O-GlcNAcylation修饰;三是OGT介导Cathepsin B的O-GlcNAcylation修饰可以维持高水平的成熟体Cathepsin B;四是TAM分泌的Cathepsin B促进肿瘤细胞的侵袭转移和化疗抵抗。
该研究的创新性及生物学意义主要包括:第一,首次揭示了TAM竞争性摄取葡萄糖的病理意义,即TAM竞争性摄取葡萄糖促进HBP和OGT介导的Cathepsin B的O-GlcNAcylation修饰及后续的成熟和分泌,进而促进肿瘤的转移和化疗抵抗;这一发现进一步揭示肿瘤免疫代谢和肿瘤免疫逃逸的新型机制,有助于设计针对TAM葡萄糖吸收、O-GlcNAcylation修饰的肿瘤治疗方法。第二,发现溶酶体定位的OGT可以修饰包括半胱氨酸蛋白酶之类的靶蛋白而调控了溶酶体在肿瘤转移与化疗抵抗中的作用,该发现拓展了我们对OGT、溶酶体生物学功能的认识。第三,首次揭示了翻译后修饰对溶酶体半胱氨酸蛋白酶蛋白水平的调控,有助于进一步探索特殊蛋白在溶酶体中稳定存在的分子机理。总之,在该研究中,研究团队首次阐明了TAM,尤其是M2样TAM竞争性摄取和利用葡萄糖对于塑造细胞特异性促肿瘤功能的重要意义,为肿瘤治疗提供了潜在的靶点。
该研究得到国家自然科学基金项目(81922032, 81788101, 31900660)、中国科协青年人才托举工程(2018QNRC001)和中国医学科学院医学与健康科技创新工程(2021-I2M-1-017)的支持。基础医学研究所曹雪涛院士和海军军医大学医学免疫学国家重点实验室张迁教授为论文的共同通讯作者,基础医学院博士后史青竹和海军军医大学医学免疫学国家重点实验室沈奇骢副教授为论文的共同第一作者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#cancer cell#
53
#Cell#
41
#CEL#
39
#肿瘤转移#
0
#曹雪涛#
42