DCR:超低位直肠癌括约肌间切除术后永久性造口的累积发生率及危险因素分析
2022-02-17 MedSci原创 MedSci原创
结肠直肠癌(carcinoma of colon and rectum)胃肠道中常见的恶性肿瘤,早期症状不明显,随着癌肿的增大而表现排便习惯改变、便血、腹泻、腹泻与便秘交替、局部腹痛等症状。
括约肌间切除术(ISR)已被越来越多地用作治疗超低位直肠癌(uLRC)患者的保留括约肌功能的最后一道防线,其肿瘤学和患者的生活功能效果是被普遍接受。然而,永久造口(PS)是这个手术的意外的后果,不能完全的避免。直肠癌患者在行低位前切除术(Low anterior resection, LPS)后有2.9%至32%的几率会出现造口。ISR手术需要经肛门分割直肠远端,部分或全部切除肛门内括约肌(IAS),并通过缝合结肠肛门来保持肠道的连续性。ISR是否会导致比低位切除术(LAR)更高的PS风险目前还不清楚,因此,本项研究目的是确定超低位直肠癌括约肌间切除术后永久性造口的累积发病率和危险因素。
本研究是对在中国火箭军特色医学中心结直肠外科的前瞻性的临床数据进行的回顾性分析。共纳入 2011 年至 2019 年连续接受括约肌间切除伴回肠造口术的 185 例患者。主要观察结果是永久性造口的发生率和危险因素。次要结果包括部分、次全和全括约肌间切除术患者之间造口几率的差异。
在随访 40 个月后,185 名患者中有 26 名患者最终需要永久性造口,5年累积发病率达17.4%。造成永久性造口的原因依次为吻合口并发症(46.2%,12/26)、疾病局部复发(19.2%,5/26)、肿瘤远处转移(19.2%,5/26)、大便失禁(3.8%,1/26)、围手术期死亡(3.8%,1/26),患者拒绝(3.8%,1/26),患者一般情况不佳(3.8%,1/26)。尽管永久性造口的发生率在括约肌间切除组之间存在显着差异(部分 vs 次全 vs 全部:8.3% vs 20% vs 25.8%,p = 0.02),但这并不是造口形成的独立预测因素。多变量分析表明吻合口漏 (OR = 5.29; p= 0.001)和吻合口狭窄(OR = 5.13;p = 0.002)独立的预测永久性造口的危险因素。
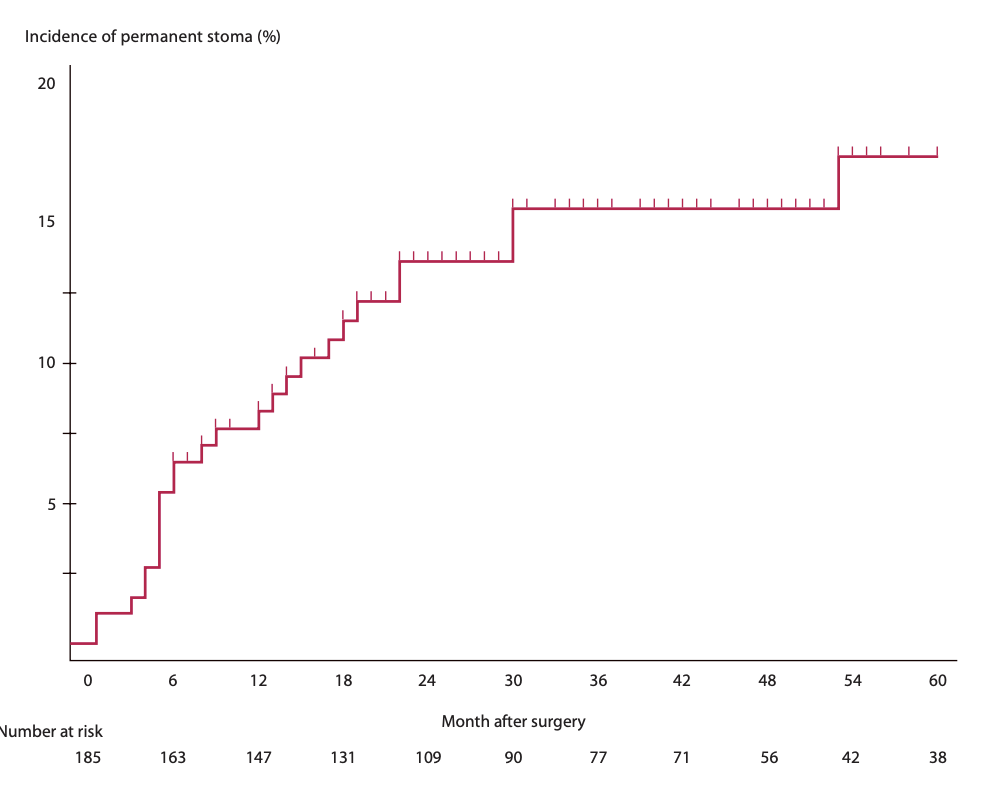
图:永久性造口随时间的变化
本项研究结果证实超低位直肠癌括约肌间切除术后永久性造口5年累积发生率为17.4%。吻合口并发症被确定为危险因素。因此,在考虑最终保留括约肌的手术时,应告知患者风险和益处。最好通过进一步减少吻合口并发症来降低永久性造口的可能性。
原始出处:
Zhang, Bin. Et al. Cumulative Incidence and Risk Factors of Permanent Stoma After Intersphincteric Resection for Ultralow Rectal Cancer. Diseases of the Colon & Rectum.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#发生率#
60
#切除术#
51
很好
54
好
60