Indian J Dent Res:猪胶原基质联合冠向瓣治疗Miller I型和II型牙龈退缩
2020-08-20 MedSci原创 MedSci原创
牙周整形手术的主要目标是获得完整的牙根覆盖(CRC)和最佳外观。本研究旨在评估3D猪胶原基质(PCM)与冠向瓣(CAF)在治疗Miller I型和II型牙龈退缩(GR)方面的有效性。
牙周整形手术的主要目标是获得完整的牙根覆盖(CRC)和最佳外观。本研究旨在评估3D猪胶原基质(PCM)与冠向瓣(CAF)在治疗Miller I型和II型牙龈退缩(GR)方面的有效性。
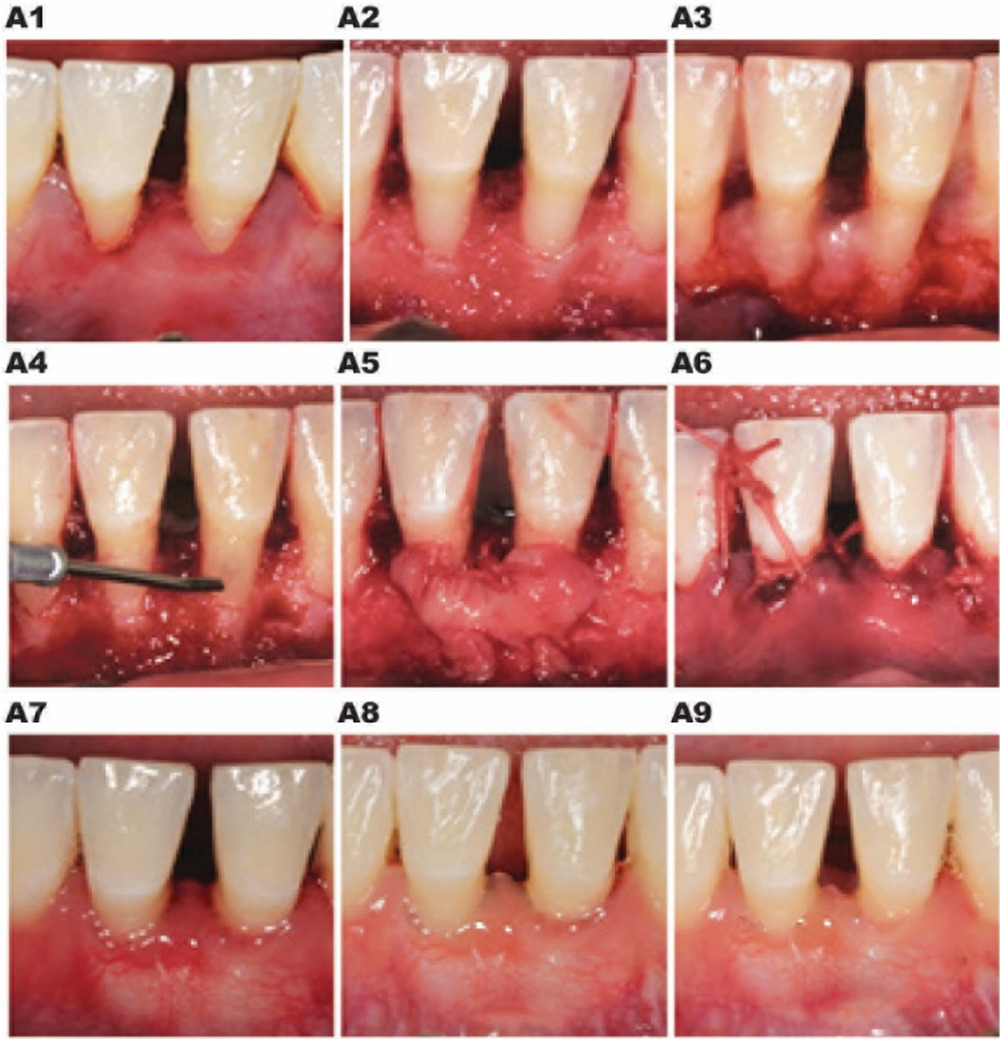
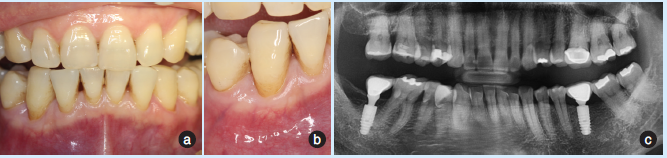
研究共纳入20例患者,有40处Miller I型和II型GR。将患者随机分为试验组(PCM + CAF)和对照组[结缔组织移植物(CTG + CAF)]。在基线和12个月后评估临床参数,如牙龈退缩深度(RD)、探诊深度、临床附着水平(CAL)和角化牙龈宽度(WKG)。在手术后12个月评估牙根覆盖率(RC%)和CRC。统计学分析采用独立t检验进行组间比较。统计学意义设定为0.05。
结果显示,试验组12个月的平均RD为0.20mm,对照组为0.12mm,而PCM+CAF的平均RC%为94.22%,CTG+CAF为96.48%。CTG+CAF的CRC较高,为80%。试验组和对照组CAL增益分别为2.05和2.07mm。WKG在试验和对照部位的增益分别为1.35和1.30mm。两组患者术后12个月的审美满意度相当。

综上所述,在本研究的范围内,使用PCM+CAF治疗GR是一种成功而有效的治疗方案,可以作为CTG的替代方案。
原始出处:
Haydar Barakat, Suleiman Dayoub, et al., Treatment of miller type I and II gingival recession defects using three-dimensional porcine collagen matrix with coronally advanced flap: A randomized clinical split-mouth trial (a 1-year follow-up). Indian J Dent Res. Mar-Apr 2020;31(2):209-216. doi: 10.4103/ijdr.IJDR_897_18.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#基质#
44
#胶原基质#
50
#DIA#
41
#牙龈退缩#
59
#IND#
50
#猪#
55