Cell突破丨颠覆传统的智能化细胞筛选技术—流式细胞仪迈入二维时代
2018-08-28 老冰 BioArt
了解细胞巨大的异质性是生物学的一个基本挑战。细胞的组成、结构和形态的差异与它们的生理功能息息相关,细胞几何结构(如大小、形状)影响着细胞内信号传导并调节细胞生长和分化,还有像细胞核形状、核质比、细胞骨架结构等一系列细胞形态上的特征,都可能和独特的细胞功能相关。在揭示这些重要的关联性问题上,需要快速搜索和分选出大型异质细胞群中具有独特化学和形态特征的细胞。
传统的细胞分选技术需要在图像数据的体积和复杂性(与精度相关)以及数据传输和图像处理速度(与响应时间相关)之间权衡,在上述问题上很难有质的突破,例如:高通量细胞分选技术如荧光激活细胞分选(FACS)只能处理低分辨率数据;基于图像的高含量筛选(High-content screening, HCS)和成像流式细胞术(imaging flow cytometry)可以进行高分辨率图像数字分析和对高维数据的机器学习,但因为数据传输和图像处理的速度有限,无法实现实时驱动。
8月27日,东京大学化学系Keisuke Goda课题组等在Cell上在线发表了题为Intelligent Image-Activated Cell Sorting的论文,提出了一种颠覆传统架构的机器智能技术——智能图像激活细胞分选仪(intelligent image-activated cell sorter , 以下简称“智能IACS”),以前所未有的速度实现了基于图像的细胞实时智能分选。与传统的流式细胞仪分析不同,细胞可以根据空间和形态学从大的异质群体中分类,对诸如细胞内蛋白质定位和细胞- 细胞相互作用的不同都可以作为参考。
研究者在一个软硬件结合的数据管理基础设施上,运行电信级10-Gbps全互联网协议(IP)架构,集成高通量细胞显微、聚焦和分类功能,实现了数据采集、处理、决策和驱动的实时自动化操作。在这个集“光学-微流体-电气-计算-机械”于一体的系统中,即使是使用深度学习算法,也能在32毫秒内实现高灵敏度、高延展性和自动化的操作,可以以每秒约100个单元的前所未有的速度进行实时图像的智能单元搜索和排序。
研究者验证了智能IACS的基本性能:1:1混合的3mm、6mm粒子的分选实验表明,基于经典算法和卷积神经网络(CNN,convolutional neural network)的小粒子富集纯度分别达到了98.6%和99.1%;生物学场景下的性能验证则通过1:19的3mm、6mm粒子分选实验实现,其小粒子富集的结果表明经典图像分析算法的通量、产量和纯度分布高达106.4eps、67.7%和96.2%。研究者通过这些实验优化了智能IACS的设置,从而可以获得更高的纯度和产量。
从某种意义上看,智能IACS是FACS的成像版本,它在技术和应用方面提供了更多功能。从微生物学到血液学领域,智能IACS对不同类型细胞的成像能力也在这项工作中得以展示。
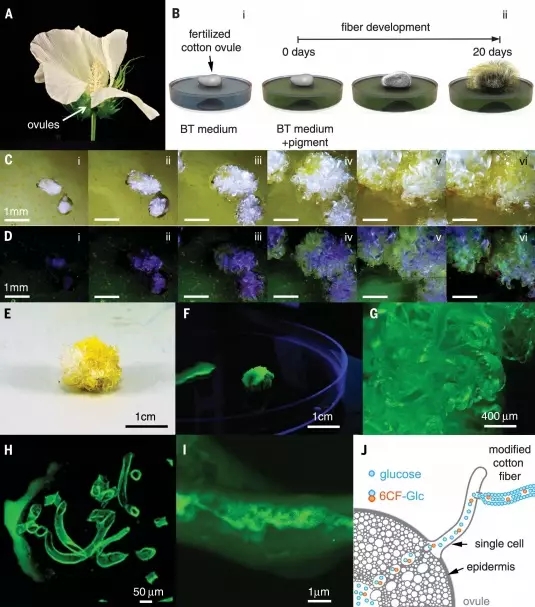
核酮糖1,5-二磷酸羧化酶/氧化酶(Rubisco)是卡尔文循环中用于光合作用CO2固定的关键酶。为了提高Rubisco在水环境中原本极低的CO2催化亲和力和扩散速率,大多数水生光合生物拥有一种生物物理学的碳浓缩机制(carbon-concentrating mechanism , CCM)。在莱茵衣藻(Chlamydomonas reinhardtii, C. reinhardtii)中,CCM的运转主要包括由钙结合蛋白CAS调控的活性碳酸氢盐(HCO3-)摄取、碳酸酐酶将HCO3-转化为CO2,以及在一种非膜结合的亚细胞器pyrenoid中Rubisco附近CO2浓度的升高。除了这些CCM相关的成分外,低CO2诱导蛋白B(LCIB)在CCM藻类中高度保守,在CCM运转过程中起关键作用。当CCM被完全诱导时,LCIB响应于降低的CO2浓度,通常会从叶绿体中的分散状态转变到类黄酮附近的环状结构。
这项工作中,研究者使用智能IACS对低CO2条件下LCIB定位异常的C.reinhardtii突变体进行了分类。实验特别使用了莱茵衣藻菌株BC-9(一个与荧光蛋白Clover融合表达LCIB的转基因品系)作为样品(STAR方法)。LCIB在叶绿体中分散的定位和在pyrenoid附近聚集的两种模式,通过FDM图像中细胞内LCIB-Clover荧光信号的变异系数(CV)得以区分。高CV值的细胞显示出LCIB-Clover蛋白在pyrenoid周围的定位,低CV值细胞显示该蛋白的分散分布模式。智能IACS在221,947次判断中分选出2,021个低CV(CV值小于1%的细胞群)细胞,研究者随后将其中的60个细胞培养并获得44个克隆,最终在31个(70%)克隆中观察到叶绿体中分散的LCIB定位。未来对分选细胞的分子生物学分析可以进一步鉴定CCM的相关基因和调节通路,从而加强对CCM这一提高合成微藻光合效率的关键机制的理解。
动脉粥样硬化血栓形成相关疾病,包括急性冠状动脉综合征和急性缺血性中风,与血小板的活化有关。这类疾病由动脉粥样硬化斑块破坏,和紧接的血小板活化引发,血小板聚集体可引起局部闭塞或末梢栓塞。因此,评估外周血中活化的血小板可用于预测和评估该疾病的状态。最近的研究结果表明,由中性粒细胞、单核细胞和血小板组成的免疫血栓(immunothrombosis)经先天免疫系统引发,可促进动脉和(/或)静脉血栓的形成。由于血小板对化学和机械刺激敏感,容易在体外自发激活,传统的全血流式细胞仪(Whole-blood flow cytometry)使用血小板活化标记物抗体,背景噪音大,无法准确检测活化的血小板。不染色的条件下检测和分离固定血液中活化的血小板(例如,血小板聚集体),在动脉粥样硬化血栓形成的准确诊断和抗血小板治疗的监测等临床应用上具有较高潜力。
智能IACS用八层的深度卷积神经网络(CNN)实现了对人血液中血小板聚集体的分选。CNN计算出图像视野中白细胞、血小板聚集体等目标识别物的概率,甚至可以将单个血小板区分出来。基于门控策略(gating strategy),血小板聚集体的监测达到了99.0%的高特异性、82.0%的高灵敏度和79.5%的高分选纯度。CNN对于血小板聚集体的高纯度的分选性能,是FACS或者基于经典图像分析的智能IACS达不到的。后续通过转录组、蛋白质组和代谢组学的分析手段对分选的血小板的进一步研究,可以确定血小板活化敏感性的关键因素,促进抗血小板新药的开发。
基于细胞内蛋白质定位和大型异质细胞群的胞间相互作用,智能IACS实现了对微藻和血细胞的实时分选,前者可以应用于光合作用相关研究,后者用于探究动脉粥样硬化血栓的形成。在未来,智能IACS的应用还可能超越研究者演示的单细胞悬浮液和细胞簇的分析、分离:只需改变流动通道和光学系统,可以进一步实现对更大型的生物体的分选,例如细胞球状体(cell spheroids)、类器官(organoids)、组织碎片或者可能是整个生物体(如果蝇胚胎,斑马鱼等)。智能IACS平台的灵活性高、可扩展性强:其功能在成像方法、传感器等方面还可以进一步增强;或可将其与高通量单细胞分析工具无缝集成,以简化与形态学表型相关的分子基础识别;对深度CNN的不断训练,则将进一步提高识别稀有细胞(如循环肿瘤细胞,抗原特异性T细胞,癌症干细胞)的准确性。总之,智能IACS的潜在应用市场是巨大的,它有望助力生物、制药和医学科学领域产生新的科学发现。
该研究由50多位不同领域的科学家合力完成。据phys.org网站报道,智能IACS的设计花了2年时间,子系统开发也需要2年时间,另外的2年时间将它们整合在一起并在微藻和血细胞样本上进行测试分析。据了解,该系统平台由于庞大而复杂,短期内还无法处理更大的生物体。
该论文的通讯作者Keisuke Goda(合田圭介,先后在UC伯克利以及MIT学习,物理学博士,UCLA的博后,激光干涉仪引力波天文台(LIGO)科学合作组织成员之一,现为东京大学物理化学系教授 )表示,他们的目标是要将过往传统的一维流式细胞仪扩展到二维,这将会有助于解决新的基础生物学问题,例如可以寻找一些影响细胞内各种不同的分子在空间定位的基因并研究其功能、研究细胞空间结构与生理功能之间的关系等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#智能化#
0
#Cell#
31
#二维时代#
28
#CEL#
23
#筛选#
0
流式细胞仪进展。
55