CHEST:FEV1的改善与减少COPD急性加重密切相关!
2017-05-10 MedSci MedSci原创
目前,临床使用的各类药物降低COPD加重风险的机制尚不清楚。近期,一项发表在杂志CHEST上的研究评估了通过1秒用力呼气量(FEV1)检测的气道通畅改善水平是否与疾病的急性加重风险降低相关。通过系统评估,研究者们确定了治疗前FEV1(dFEV1)的变化和中度至重度COPD急性发作的频率。使用Meta回归分析,研究者们生成了一个以dFEV1作为调节变量,急性加重率(RD)、恶化率(RR)或风险比(H
目前,临床使用的各类药物降低COPD加重风险的机制尚不清楚。
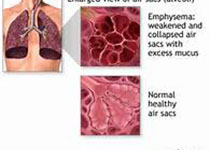
近期,一项发表在杂志CHEST上的研究评估了通过1秒用力呼气量(FEV1)检测的气道通畅改善水平是否与疾病的急性加重风险降低相关。
通过系统评估,研究者们确定了治疗前FEV1(dFEV1)的变化和中度至重度COPD急性发作的频率。使用Meta回归分析,研究者们生成了一个以dFEV1作为调节变量,急性加重率(RD)、恶化率(RR)或风险比(HR)绝对差异作为因变量的模型。
此项研究结果显示:RD和RR的分析包括119,227例患者,HR的分析共包括73,475例患者。对于每100 mL的FEV1的变化,HR降低21%(95%CI:17-26%,P <0.001,R2 = 0.85),绝对急性发病率每位患者每年减少0.06(95% CI:0.02-0.11,P = 0.009,R2 = 0.05),相当于RR为0.86(95%CI:0.81-0.91,P <0.001,R2 = 0.20)。在多个亚组分析中,这种与急性加重的风险相关性仍然具有统计学意义。
此项研究所示的FEV1的增加与COPD急性加重风险降低之间的显着相关性表明,气道通畅是造成这种效应的重要机制。
原始出处:
Zider AD, Wang X, et al. Reduced COPD exacerbation risk correlates with improved FEV1: A meta-regression analysis. Chest. 2017 May 5. pii: S0012-3692(17)30817-6. doi: 10.1016/j.chest.2017.04.174.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#EST#
39
#急性加重#
0
#FEV1#
35
#Chest#
30
#FEV#
39
学习了,谢谢作者分享!
49
学习了,很好,谢谢!
44
认真学习,值得推崇
47