Thorax:COPD患者抗衰老因子-生长分化因子11减少!
2017-04-29 xing.T MedSci原创
由此可见,GDF11的减少可能参与了COPD患者肺脏中的细胞衰老。
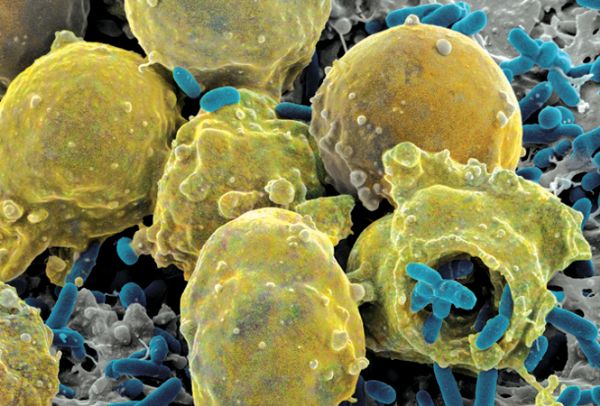
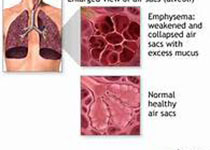
慢性阻塞性肺病(COPD)患者的肺脏中可以观察到细胞衰老,并可能参与了疾病的发病机制。生长分化因子11(GDF11)属于转化生长因子β超家族的成员,最近有研究报道小鼠中GDF11是一种具有重返年轻效应的循环蛋白质。近日,胸部疾病领域权威杂志Thorax上发表了一篇研究文章,研究人员旨在探讨COPD患者肺脏中血浆中GDF11的数量,并且阐明GDF11在细胞衰老中可能发挥的作用。
在两个独立的队列中,研究人员采用Western蛋白印迹方法检测了血浆中GDF11的浓度,分别采用免疫组织化学和定量反转录PCR的方法检测了肺脏中GDF11的定位和表达。研究人员在体外观察了GDF11对香烟烟雾提取物(CSE)诱导的细胞衰老的影响,以及体内观察了GDF11对弹性蛋白酶诱导的细胞衰老的影响。
研究人员发现在两个独立的队列中COPD患者血浆中GDF11的水平相比于对照者明显下降。血浆中GDF11水平与肺功能数据呈显著的正相关。在COPD患者间充质细胞中GDF11的mRNA水平表达降低。慢性暴露于CSE可以降低GDF11的表达。在体外实验中,采用GDF11处理可以显著抑制CSE诱导的细胞衰老和炎症介质的表达上调,部分是通过Smad2/3信号。每日采用GDF11治疗可以减缓弹性蛋白酶诱导的肺气肿动物模型细胞衰老和空隙扩大。
由此可见,GDF11的减少可能参与了COPD患者肺脏中的细胞衰老。
原始出处:
Katsuhiro Onodera, et al. Decrease in an anti-ageing factor, growth differentiation factor 11, in chronic obstructive pulmonary disease.Thorax. 2017. http://dx.doi.org/10.1136/thoraxjnl-2016-209352
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抗衰老因子#
33
学习了,谢谢作者分享!
71
学习了,谢谢作者分享!
86
#COPD患者#
30
学习了谢谢分享
68