JACC:肠道胆固醇吸收率低的血透患者更能获益于阿托伐他汀治疗
2015-06-03 张旭栋译 MedSci原创
瑞士伯尔尼大学Silbernagel G等人研究了血透患者中,肠道胆固醇的吸收率与阿托伐他汀治疗的收益率相关性,其研究成果发表在6月份Journal of the American College of Cardiology期刊上。 背景:血液透析患者肠道胆固醇的吸收高;相对于其他他汀治疗(抑制胆固醇合成)患者而言,其他汀受益率较低。 目的:本研究旨在探讨个体胆固醇的吸收率是否会影响阿托伐他汀
瑞士伯尔尼大学Silbernagel G等人研究了血透患者中,肠道胆固醇的吸收率与阿托伐他汀治疗的收益率相关性,其研究成果发表在6月份Journal of the American College of Cardiology期刊上。
背景:血液透析患者肠道胆固醇的吸收高;相对于其他他汀治疗(抑制胆固醇合成)患者而言,其他汀受益率较低。
目的:本研究旨在探讨个体胆固醇的吸收率是否会影响阿托伐他汀的有效性,从而探讨其对血透患者心血管疾病的危险影响。
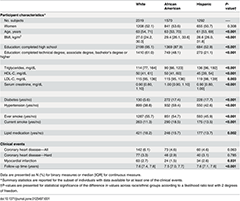
方法:研究纳入了1,030例德国糖尿病血透研究(4D)的患者,将其随机分配到20毫克阿托伐他汀治疗组(N =519)或安慰剂组(n=511)。主要终点是复合心血管事件。次要终点包括全因死亡率和所有心脏事件。三分位数胆甾烷醇/胆固醇比例,作为胆固醇吸收的一个生物标志物,被用来测定胆固醇吸收的高低。
结果:共有454例患者发生主要终点事件。生存曲线分析显示,三分位数与阿托伐他汀治疗之间的关联:显著提高主要终点事件风险。胆甾烷醇/胆固醇比例的三分位数证实了这种效果:第一个三分位数显示阿托伐他汀能减少主要终点事件的风险(风险比HR:0.72; P = 0.049),但不包括第二个三分位数(HR:0.79 ; P =0.225)或第三个三分位数(HR:1.21; P =0.287)。阿托伐他汀仅在第一个三分位数上能显著降低全因死亡率和所有心脏事件的风险。
结局:肠道胆固醇的吸收,通过胆甾烷醇/胆固醇的比例反映,能够预测阿托伐他汀的有效性(减少血液透析患者的心血管风险)。那些胆固醇吸收率低的患者能从阿托伐他汀治疗中受益,而那些胆固醇吸收率高患者却并不能显著受益。
原文出处:
Silbernagel G, Fauler G, Genser B, et al. Intestinal cholesterol absorption, treatment with atorvastatin, and cardiovascular risk in hemodialysis patients. Journal of the American College of Cardiology. 2015;65(21):2291-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
28
收藏
102
#ACC#
34
#血透#
29
收藏下先
108