Lancet Infect Dis:全球目前有超过230万艾滋和丙肝的共感染患者
2016-03-11 佚名 生物谷
近日,一项来自布里斯托大学等机构的研究人员发现,目前全球大约有230万HIV感染者同时还是丙肝感染者(HCV),相关研究刊登于The Lancet Infectious Diseases杂志上。其中有超过一半患者(130万左右)都是注射吸毒者,本文研究发现,相比未感染HIV的个体而言,感染HIV的个体发生丙肝感染的可能性是前者的6倍,这就提示卫生组织个改善HIV/HCV共感染者的相应治疗政策。
近日,一项来自布里斯托大学等机构的研究人员发现,目前全球大约有230万HIV感染者同时还是丙肝感染者(HCV),相关研究刊登于The Lancet Infectious Diseases杂志上。其中有超过一半患者(130万左右)都是注射吸毒者,本文研究发现,相比未感染HIV的个体而言,感染HIV的个体发生丙肝感染的可能性是前者的6倍,这就提示卫生组织个改善HIV/HCV共感染者的相应治疗政策。
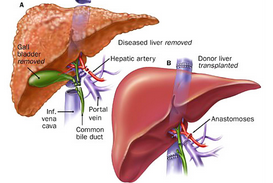
目前HIV和HCV感染是全球主要的健康问题,全世界大约有370万HIV感染者,同时大约有1.15亿慢性HCV患者,然而此前很少有研究进行HIV/HCV共感染的研究,本文研究或是首次对HIV/HCV共感染进行的相关研究。文章中研究者对783项医学研究进行回顾来对患者HIV/HCV共感染进行有效评估,研究者Philippa Easterbrook说道,本文研究不仅揭示了HIV患者感染HCV风险较高,而且还说明注射吸毒人群中发生着HCV的高度流行,至少在80%以上,因此这就需要扩大常规对HIV患者进行HCV感染的检测,尤其是高风险的个体,同时也应当开发新型高治愈性的HCV疗法。
研究者Lucy Platt表示,改善对HCV和HIV患者的监督可以有效帮助解释两种病毒共感染的机体,并且为开发新型的检测、预防及相关疗法提供帮助。本文研究揭示了注射毒品如何驱动HIV感染者中HCV的流行,尤其是东欧及中亚国家人群;同时研究者还提出了需要扩大预防性的干预策略,比如针头、注射器以及阿片替代疗法等,其都可以有效降低共感染的发生。
本文研究重点关注了HCV抗体的流行,即研究者测定了HCV的暴露但并不测定病毒的活动性感染情况,测定活动性病毒的存在以及对疗法的需求或许需要更加昂贵的病毒检测技术,大约有20%-30%暴露于HCV的个体在后期机体的抗体会自动清除病毒。文章中研究者揭示了HIV/HCV共感染对东欧及中亚国家的巨大负担,据估计在这些地区有607700名共感染患者(27%的比例),尤其是在注射吸毒者中居多,撒哈拉沙漠以南非洲地区占到了所有病例中的19%,大约429600个共感染者。
原始出处:
Dr Lucy Platt, Philippa Easterbrook, et al,Prevalence and burden of HCV co-infection in people living with HIV: a global systematic review and meta-analysi,Lancet Infect Dis,2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Dis#
32
#共感染#
31
#Lancet#
23
未来的方向,不知道是否会进一步发展
117
未来的方向,不知道是否会进一步发展
110
未来的方向,不知道是否会进一步发展
146
这么多人
110
好好学习
115
珍爱生命吧!
79