BMC Cancer:好消息!UPLC-MS血液脂类分析可早期诊断肝癌!
2015-12-21 Seven L 译 MedSci原创
慢性乙型病毒性肝炎 (CHB) 病毒感染是肝细胞性肝癌(HCC)的主要病因,若不能早诊断HCC,患者预后将会非常糟糕。目前临产上迫切需要能够对对于HCC做出早期精确诊断的生物标志物。研究者进行了一项研究,探究血液中有没有可以作为诊断乙肝相关HCC的潜在标志物。该研究纳入了32名HCC患者,30名肝硬化(LC)患者,25名CHB患者,还有34名健康人群。使用UPLC-MS分析参与者血液中脂类组学情况
慢性乙型病毒性肝炎 (CHB) 病毒感染是肝细胞性肝癌(HCC)的主要病因,若不能早诊断HCC,患者预后将会非常糟糕。目前临产上迫切需要能够对对于HCC做出早期精确诊断的生物标志物。研究者进行了一项研究,探究血液中有没有可以作为诊断乙肝相关HCC的潜在标志物。
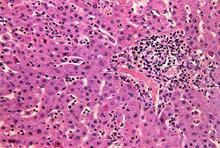
该研究纳入了32名HCC患者,30名肝硬化(LC)患者,25名CHB患者,还有34名健康人群。使用UPLC-MS分析参与者血液中脂类组学情况。
研究数据显示,基于UPLC-MS检测血液中脂类,对于LC患者,该检测比常用的AFP在诊断LC上会更精确。该方法从LC患者中区分HCC患者的敏感性为78%,特异性是64%;而AFP的敏感性和特异性分别为38%和93%。使用UPLC-MS方法区分CHB和HCC的敏感性和特异性均为100%。
研究结果表明,对HCC高危人群进行基于UPLC-MS方式的血液脂类组学分析,可有效且方便的诊断HCC。
原始出处:
Passos-Castilho AM, Carvalho VM,et al.Serum lipidomic profiling as a useful tool for screening potential biomarkers of hepatitis B-related hepatocellular carcinoma by ultraperformance liquid chromatography-mass spectrometry.BMC Cancer. 2015 Dec 18;15(1):985.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#BMC#
24
需要看下原文
122
这个不错
96
赞
107
有意思!下载原文看看!
110
#早期诊断#
27