盘点:2016年结直肠癌重要研究成果一览
2016-08-25 MedSci MedSci原创
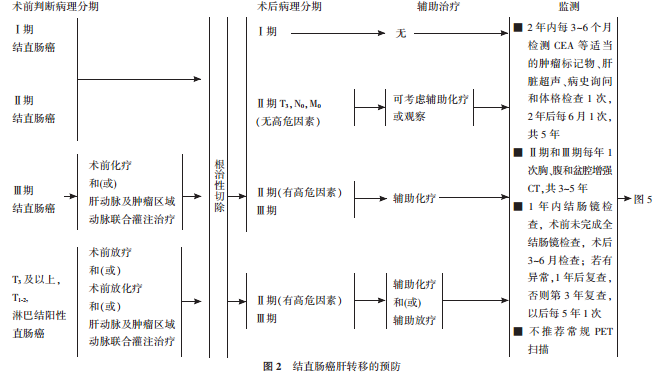
近期结直肠癌研究领域的大量基础和临床研究,从不同方向、不同角度对乳腺癌及其并发症的临床诊治进行了深入研究,为结直肠癌的临床管理寻找最新方向。梅斯医学小编,之前为大家盘点过“2016结直肠癌重要指南共识汇总”的文章,那么梅斯医学小编就近期结直肠癌领域重要研究成果进行回顾。【1】Gut:ω- 3多不饱和脂肪酸大量摄入可能降低结直肠癌死亡风险BMJ旗下著名期刊Gut 近日发表一篇文章,探究了结直肠癌

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研究成果#
43
学习一下,好
36
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
42
好,太赞了,归纳的太好了,小编辛苦了
40
#结直肠#
40
先下手为强?,学习学习,参考相关知识
41
学习起来
46
学习了,赞一个!!!
16
学习了,赞一个!!!
24
继续学习
18