PNAS:陈赛娟白血病治疗药物毛萼乙素在自身免疫病领域研究获进展
2013-04-01 中科院上海生命科学研究院 中科院上海生命科学研究院
中科院上海生命科学研究院/上海交通大学医学院健康科学研究所、上海交通大学医学基因组学国家重点实验室/上海血液学研究所陈赛娟院士领衔的科研团队用中药提取物毛萼乙素治疗自身免疫性疾病多发性硬化症(Multiple Sclerosis,MS)取得新突破,研究成果发表在国际权威学术期刊《美国科学院院刊》(Proceedings of the National Academy of Sciences of

中科院上海生命科学研究院/上海交通大学医学院健康科学研究所、上海交通大学医学基因组学国家重点实验室/上海血液学研究所陈赛娟院士领衔的科研团队用中药提取物毛萼乙素治疗自身免疫性疾病多发性硬化症(Multiple Sclerosis,MS)取得新突破,研究成果发表在国际权威学术期刊《美国科学院院刊》(Proceedings of the National Academy of Sciences of the United States of America)上。
MS是一种主要累及中枢神经系统的自身免疫性疾病,其病理特征为中枢神经系统炎性浸润以及白质脱髓鞘,患者多从中青年起发病,进行性瘫痪,该病在欧洲和北美地区发病率最高,已成为非外伤致残的首要病因。现有的MS标准治疗药物对于疾病的缓解程度有限,且有些副作用明显,亟待更有针对性的药物研发。
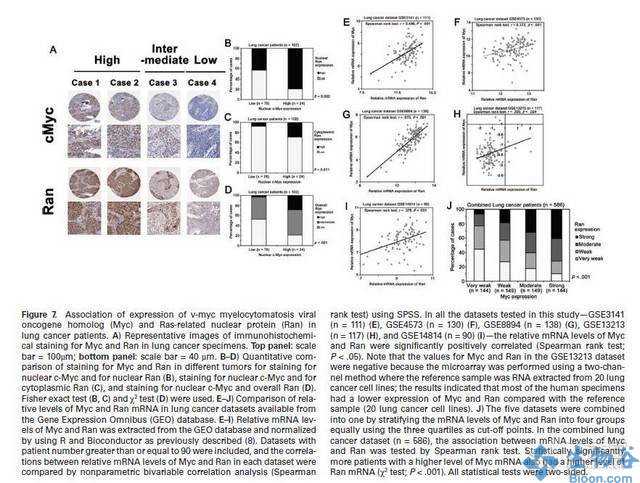
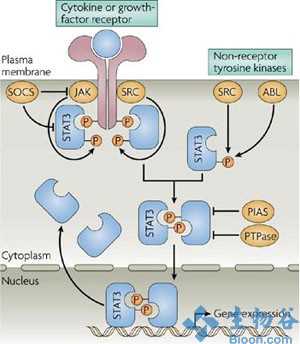
研究组前期研究结果显示,毛萼乙素可以抑制急性髓系白血病细胞内组成型活化的NF-κB信号通路,并显著延长白血病小鼠模型的生存期。同时,毛萼乙素可以通过上调活性氧(reactive oxygen species, ROS)水平来改变细胞的氧化还原状态,继而影响胞内许多对氧化应激敏感的信号通路以及转录因子的活性。基于NF-κB和ROS信号通路也参与许多自身免疫性疾病如类风湿性关节炎、系统性红斑狼疮和多发性硬化症的炎症反应,在此项研究中,研究人员利用MS的疾病模型小鼠实验性自身免疫性脑脊髓炎(experimental autoimmune encephalomyelitis, EAE)进一步探索了毛萼乙素潜在的抗炎性质。研究发现,毛萼乙素给药可有效缓解小鼠的EAE病情,减轻其脊髓病灶部位的炎性浸润和脱髓鞘病变。自身抗原反应性淋巴细胞经毛萼乙素处理后,失去过继移植的致病能力。机制研究显示,毛萼乙素通过阻滞异常活化的JAK/STAT,NF-κB信号通路以及上调ROS水平,选择性地抑制了EAE小鼠体内致病性Th1和Th17细胞的分化和增殖,从而起到缓解疾病的作用。这些研究结果提示,毛萼乙素在自身免疫等炎性疾病中可能也具有良好的应用前景。(生物谷Bioon.com)

doi:10.1073/pnas.1222863110
PMC:
PMID:
Bo Jiaoa,1, Zhi-Hong Rena,b,1, Ping Liua,1, Li-Juan Chena,c,1, Jing-Yi Shia, Ying Donga, Julien Ablaind, Lin Shia, Li Gaoa, Jun-Pei Hub, Rui-Bao Rena, Hugues de Théd,e, Zhu Chena,e,2, and Sai-Juan Chena,e,2
The refractoriness of acute promyelocytic leukemia (APL) with t(11;17)(q23;q21) to all-trans retinoic acid (ATRA)-based therapy concerns clinicians and intrigues basic researchers. By using a murine leukemic model carrying both promyelocytic leukemia zinc finger/retinoic acid receptor-α (PLZF/RARα) and RARα/PLZF fusion genes, we discovered that 8-chlorophenylthio adenosine-3′, 5′-cyclic monophosphate (8-CPT-cAMP) enhances cellular differentiation and improves gene trans-activation by ATRA in leukemic blasts. Mechanistically, in combination with ATRA, 8-CPT-cAMP activates PKA, causing phosphorylation of PLZF/RARα at Ser765 and resulting in increased dissociation of the silencing mediator for retinoic acid and thyroid hormone receptors/nuclear receptor corepressor from PLZF/RARα. This process results in changes of local chromatin and transcriptional reactivation of the retinoic acid pathway in leukemic cells. Meanwhile, 8-CPT-cAMP also potentiated ATRA-induced degradation of PLZF/RARα through its Ser765 phosphorylation. In vivo treatment of the t(11;17) APL mouse model demonstrated that 8-CPT-cAMP could significantly improve the therapeutic effect of ATRA by targeting a leukemia-initiating cell activity. This combined therapy, which induces enhanced differentiation and oncoprotein degradation, may benefit t(11;17) APL patients.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究获进展#
26
#治疗药物#
28
#陈赛娟#
31
#PNAS#
26
#免疫病#
37
#自身免疫病#
32
但离临床还早
16