JAMA Neurol:这种梗死患者,双抗治疗更有效
2018-04-13 佚名 天坛会
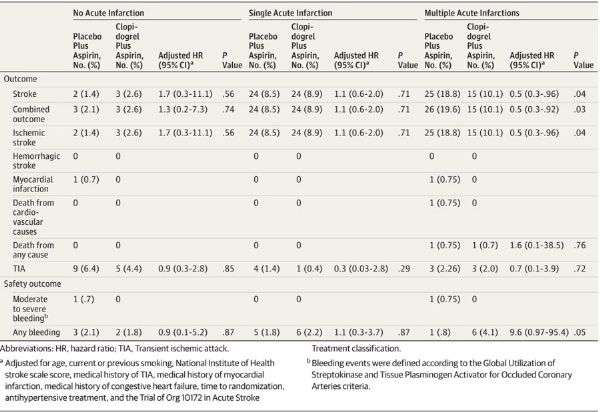
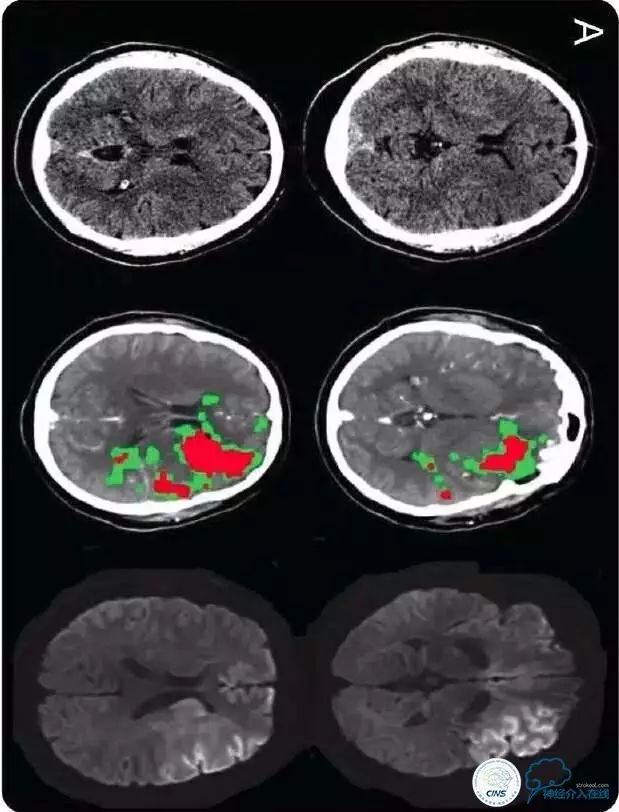
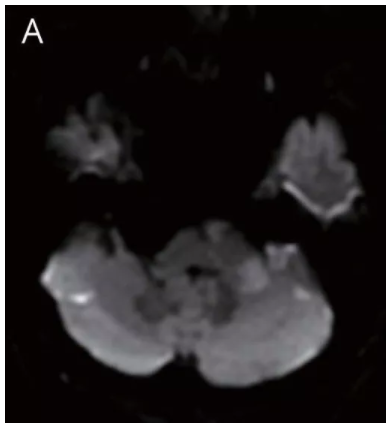
来自北京天坛医院的Jing Jing等通过CHANCE研究亚组分析表明,脑梗死模式能有效地将非心源性短暂性脑缺血发作(TIA)或轻型脑卒中患者3个月内卒中复发风险分层,并且多发急性梗死(MAIs)患者可以从双重抗血小板治疗中获益。该研究发表在近期的JAMA Neurology杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
0
学习了谢谢分享!!
55
#双抗治疗#
35
#双抗#
41
了解了
70