Neurology:ASPECTS评分和CT灌注哪一个更**?
2017-11-30 杨中华 首都医科大学附属北京天坛医院
作者 杨中华 首都医科大学附属北京天坛医院 大面积梗死的患者经过再灌注治疗往往预后不良,甚至再灌注性水肿或出血。ASPECTS评分是一项10分评分系统,评价平扫脑CT预先设定前循环区域的脑实质低密度作为早期缺血性特征。在几项大型急性缺血性卒中血管内治疗的随机临床试验中,采用这项评分标准作为影像学纳入标准。ASPECTS评分能够识别哪些急性缺血性卒中能够从再灌注治疗中获益,或有害。
作者 杨中华 首都医科大学附属北京天坛医院
大面积梗死的患者经过再灌注治疗往往预后不良,甚至再灌注性水肿或出血。ASPECTS评分是一项10分评分系统,评价平扫脑CT预先设定前循环区域的脑实质低密度作为早期缺血性特征。在几项大型急性缺血性卒中血管内治疗的随机临床试验中,采用这项评分标准作为影像学纳入标准。ASPECTS评分能够识别哪些急性缺血性卒中能够从再灌注治疗中获益,或有害。
为了对比ASPECTS评分和CT灌注对急性前循环梗死大小的预测准确性,2017年6月来自澳大利亚的Jelle Demeestere等在Neurology上发表了他们的研究结果。
该观察性研究共纳入了59例急性前循环缺血性卒中的患者,这些患者都进行了平扫CT、灌注CT检查,并且CT扫描100min之内进行了MRI检查。
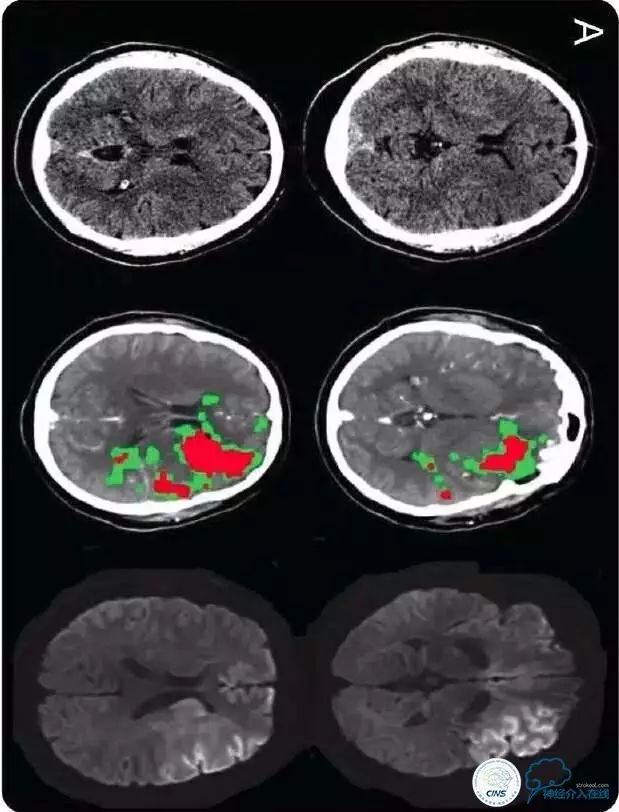
A图:ASPECTS 5分,CT灌注核心体积58ml(红色为核心、绿色为半暗带),DWI体积106ml三者的一致性:
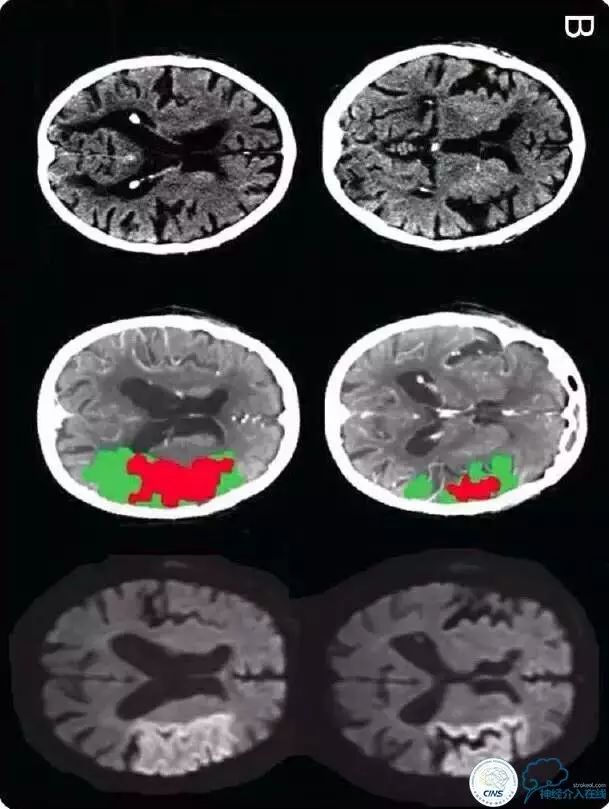
B图:ASPECTS 9分,CT灌注核心体积52ml(红色为核心、绿色为半暗带),DWI体积90ml三者的一致性:
他们发现平均ASPECTS评分未8分(IQR 5-9)。平均CT灌注核心体积为22ml (IQR 10.4-71.9)。平均MRI DWI病灶体积为24.5ml (IQR 10-63.9)。CT灌注和ASPECTS评分的精确性没有显著性差异(c statistic 0.95 vs 0.87, p value for difference = 0.17)。DWI病灶体积>=70ml的最佳ASPECTS评分cutoff值为<7(敏感性0.74,特异性0.86,Youden J = 0.6),最佳CT灌注核心体积cutoff值为>=50ml(敏感性0.86,特异性0.97,Youden J = 0.84)。
最终作者认为对于预测急性缺血性卒中超急性期MRI病灶体积,CT灌注和ASPECTS评分的精确性没有差异。
文献出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ASPECTS#
42
#Neurol#
24
#PE#
34
不错.可以借鉴学习
68
学习了.谢谢分享!
49
#CTS#
31
学习了.好文章
57
学习了新知识
56
学习了.谢谢.
54
有没有核磁灌注的相关研究呢
14