JAMA子刊:机械取栓对ASPECTS评分低分的卒中患者的结果
2022-02-20 MedSci原创 MedSci原创
超过五分之一的ASPECTS为2-5的患者在MT后实现了90天功能独立。
关于机械血栓切除术(MT)对现实世界中出现大面积核心梗死的中风患者的治疗效果,目前数据有限。为了研究大血管闭塞且ASPECTS评分为2-5分的患者进行机械血栓切除术的安全性和有效性。来自南卡罗来纳医科大学神经外科的专家开展了一项研究,结果发表在JAMA Network Open杂志上。
这项回顾性队列研究使用了来自中风血栓切除术和动脉瘤登记处(STAR)的数据,该登记处结合了美国、欧洲和亚洲的28个具有血栓切除能力的中风中心的前瞻性数据库。该研究包括颈内动脉或大脑中动脉M1段闭塞的2345名患者。患者在干预后被随访了90天。
ASPECTS是一个10分制的评分系统,基于基线无对比计算机断层扫描的早期缺血变化程度,10分表示正常。所有的患者都接受了MT。主要结果和措施是90天的良好结果(mRS评分为0-2)相关的因素,包括ASPECTS为2-5和在延长的窗口期(从症状出现的6-24小时)接受MT的交互项。
共纳入2345名接受MT治疗的患者(1175名女性[50.1%];中位年龄,72岁[IQR,60-80岁];2132名患者[90.9%]的ASPECTS≥6,213名患者[9.1%]的ASPECTS为2-5)。在90天时,213名ASPECTS为2至5的患者中,有47名(22.1%)mRS评分为0至2(25.6%[176名中的45名]的患者接受了成功的再通疗法[改良脑缺血溶栓评分≥2B],与5.4%[37名中的2名]的患者接受了不成功的再通疗法;P = 0.007)。
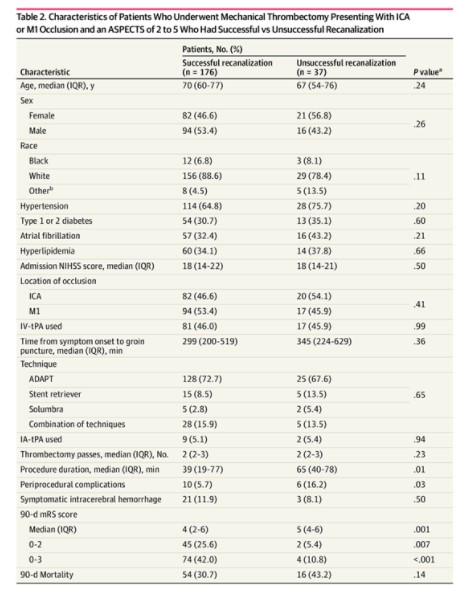
在控制了潜在的混杂因素后,低ASPECTS(OR=0.60;95%CI,0.38-0.85;P = .002)和在扩展窗口出现(OR=0.69;95%CI,0.55-0.88;P = .001)与较差的90天结果有关,这两个因素之间没有明显的交互作用(P = .64)。
在这项队列研究中,超过五分之一的ASPECTS为2-5的患者在MT后实现了90天功能独立。低ASPECTS的患者成功再通的可能性几乎是5倍。低ASPECTS与90天结果的关系,在早期与延长的MT窗口期的病人中并无不同。
参考文献:
Outcomes of Mechanical Thrombectomy for Patients With Stroke Presenting With Low Alberta Stroke Program Early Computed Tomography Score in the Early and Extended Window. JAMA Netw Open. 2021;4(12):e2137708. doi:10.1001/jamanetworkopen.2021.37708
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASPECTS#
50
#卒中患者#
38
#PE#
38
#CTS#
36
#取栓#
37
#机械取栓#
55