Biomed Res Int:苏州医工所在低剂量CT成像研究中取得进展
2017-04-29 李铭 苏州生物医学工程技术研究所
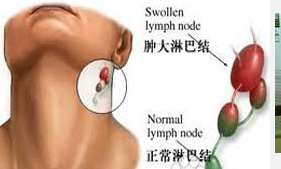
当前,随着CT断层扫描在医学诊断中的应用越来越广泛,CT成像中的低剂量成像问题已经引起了人们越来越多的关注。大量的临床实践表明超过正常范围的CT 辐射剂量与人体新陈代谢异常乃至癌症等疾病的诱发密切相关。然而,在目前的CT设备中,采用低剂量扫描协议采集到的影像会导致重建图像噪声和伪影严重,影响临床医生对异常组织的确诊率。低剂量成像协议主要包含:1)采用降采样曝光;2)采用较低的管压和管电流曝光。前者
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Bio#
25
#低剂量CT#
30
#低剂量#
28
#Med#
19
学习了 谢谢
41
学习了,谢谢
47