综述:双源CTVNC技术在诊断隐匿性骨折中的应用进展
2017-01-16 陈婷婷,刘白鹭,哈尔滨医科大学附属第二医院CT室 中国临床医学影像杂志
作者:陈婷婷,刘白鹭,哈尔滨医科大学附属第二医院CT室 隐匿性骨折是指不易被传统影像学检查方法发现而实际存在的细微骨折,临床上容易漏诊。如果诊断不及时,可能会延误治疗、影响治疗效果,若错过治疗时机可造成不可逆的局部松质骨坏死、退行性骨关节病以及骨软骨缺损等严重后果。所以提高隐匿性骨折的检出率十分必要。 隐匿性骨折(骨挫伤)由于松质骨骨小梁微观压缩断裂导致骨髓水肿(BME),
作者:陈婷婷,刘白鹭,哈尔滨医科大学附属第二医院CT室
隐匿性骨折是指不易被传统影像学检查方法发现而实际存在的细微骨折,临床上容易漏诊。如果诊断不及时,可能会延误治疗、影响治疗效果,若错过治疗时机可造成不可逆的局部松质骨坏死、退行性骨关节病以及骨软骨缺损等严重后果。所以提高隐匿性骨折的检出率十分必要。
隐匿性骨折(骨挫伤)由于松质骨骨小梁微观压缩断裂导致骨髓水肿(BME),因此可以通过检测BME来发现隐匿性骨折。BME是影像学的一个描述性术语,是由多种病因所致的非特异性表现,其中最常见的原因是创伤。继发于创伤的BME是由于骨小梁损伤导致的骨髓局部出血水肿。
BME在MRI中显示最佳,表现为骨髓内T1加权像信号强度减低、T2加权像及压脂序列(如STIR序列)信号强度增高的区域,我们可以根据这种表现检测隐匿性骨折。然而在T2加权像及STIR序列中,骨折线会被周围高信号强度的水肿掩盖,因此MRI可能更难显示骨折线。此外,MRI检查具有一些限制:检查需要很长时间,情况紧急时不适合行MRI检查;老年人常有MRI检查的禁忌症(如体内有心脏起搏器、铁磁性物质等)。
核素骨扫描(ECT)也可以检测隐匿性骨折,而且有助于排除全身性转移性疾病。但其不能显示BME,而且特异性差,空间分辨率低,辐射剂量大。此外,ECT在创伤后至少72h才能显示骨折部位的放射性浓聚,而MRI及双源CT在创伤后短时间内即可发现BME。因此ECT不适合急诊早期诊断隐匿性骨折。CT由于空间分辨率高,经常用于评估急性创伤中X线无法显示的隐匿性骨折,其强大的后处理功能可帮助判断骨折类型及骨折线涉及的范围。然而常规CT在评估BME中具有一定的限制:对于骨折线不明显的隐匿性骨折显示不清,而且通常无法判断骨折的准确时间。
双源CT可以通过检测BME来诊断隐匿性骨折,尽管其检测BME的灵敏度较MRI稍低,但具有很多优势:禁忌症少,扫描时间短,能显示细微的皮质骨折。目前双源CT在骨骼肌肉系统中的应用包括检测痛风性关节炎的关节内及关节周围是否存在谷氨酸钠尿酸盐结晶、判断BME、显示肌腱和韧带以及减少金属假体所致的硬化性伪影。
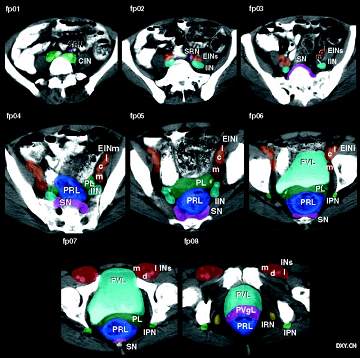
双源CT在两个固定的能量水平下持续发射X射线,对于骨骼肌肉系统,这两个能量通常设置为80kV和140kV,随后两个能量的图像分别重建。在图像重建过程中,数据迭代修正可以减少射线硬化伪影,消除射线硬化伪影在急性创伤中具有显著优势,不仅能更清晰地显示BME的范围,而且能更精确地评估损伤的严重性。
双源CT根据物质的不同化学成分在两种不同能量水平下对X射线的衰减不同(即物质分解技术)来区分不同的物质,这与被检物质的原子序数、原子量及电子密度密切相关。随着双源CT的发展,可以通过虚拟非钙质(Virtualnon-calcium,VNC)技术使BME可视化。双源CTVNC技术将松质骨中钙质信号去除,从而产生VNC图像。双源CT能够用平均CT值定量评估骨髓的变化,用VNC程序去除钙质的信号后,松质骨的平均CT值就接近骨髓成分的CT值,由于骨髓中含有丰富的脂肪,而创伤伴随的骨小梁的微小骨折、水肿及出血会引起骨髓腔内液体及血液增多,因此在正常低密度的骨髓背景下BME表现为高密度的区域。颜色编码图像及灰阶图像均可用于评估骨髓的衰减变化。此外,颜色编码图像还能帮助划定灰阶图像中发生衰减变化的区域(即感兴趣区)。
因此双源CTVNC图像能够视觉分析及定量分析BME的相关衰减变化,在临床工作中这种异常衰减的可视化分析比定量分析更简便。双源CTVNC技术的价值主要是检测CT骨三维重建图像上不易发现的骨折。双源CT可以根据骨挫伤的位置和形状来推断骨关节内部结构紊乱及相关软组织异常情况,双源CT将会成为评估创伤继发的骨关节内部结构紊乱的一种实用工具。在此过程中应仔细观察韧带损伤,因为如果出现韧带损伤,可能需要外科手术治疗。
如果在VNC图像上观察到骨挫伤伴随其他表现(如嵌插骨折、Segond骨折或关节积脂血症),可以更早地联合MRI来评估损伤程度并帮助制定外科手术计划。Ai等发现大多数骨挫伤已愈合部位的CT值不在骨挫伤部位的CT值变化范围之内,而与正常膝关节相似;因此推断如果在双源CT上看不见骨挫伤,即受损膝关节的平均CT值与对侧膝关节的4个正常部位的平均CT值无明显差异,就代表骨挫伤的消退。
MRI显示骨挫伤在创伤后4周左右开始消退,但是完全愈合需要数周至数年。研究表明双源CTVNC技术能够检测创伤后至少10周内的骨挫伤。相关研究证实双源CT已成功地显示以下几种骨折方式的BME。
1.四肢关节骨折
目前,双源CTVNC技术已成功用于评估急性膝关节损伤引起的BME。Pache等首次应用双源CTVNC技术评估急性膝关节创伤患者的骨挫伤,证实其可以检测外伤性BME,对急性创伤后怀疑前纵韧带断裂的患者也有很大帮助,颜色编码的VNC成像可以更好的观察到BME的衰减变化。相关研究表明双源CT对于检测膝关节及踝关节创伤后骨挫伤具有较高的敏感性及阴性预测值,Pache等报道敏感性为86.4%。Reagan等阐述了他们用双源CTVNC算法评估BME的最初经验,为双源CTBME重建算法诊断隐匿性骨折提供了更多依据,证实双源CT可以显示反Segond骨折、急性无移位性跟骨骨折、桡骨远端骨折中的BME。
Guggenberger等利用双源CTVNC技术检测了踝关节创伤导致的BME,报道了距骨顶部及胫骨粗隆的急性BME。
2.髋关节骨折
Reddy等证实了双源CTVNC技术的算法也能用于检测髋关节隐匿性骨折导致的BME,并认为双源CTVNC技术与其他影像学检查方法相比在诊断髋关节骨折中敏感性更高,但特异性稍低。Reddy不仅发现了预期中的大转子骨折线周围的BME,而且还观察到了股骨粗隆间无骨折线的BME。研究表明大转子骨折经常伴随股骨粗隆间骨折,然而大转子骨折只需要保守治疗,而股骨粗隆间骨折可能需要外科手术治疗。髋关节骨折如果诊断不及时,可能会合并股骨头坏死、血栓栓塞等并发症。因此,早期、准确地诊断髋关节骨折对于指导治疗及判断预后至关重要。
3.椎体压缩性骨折
椎体压缩性骨折较四肢骨骨折症状轻微,因此不易察觉,经常被临床医生及放射科医生漏诊。若不稳定的椎体压缩性骨折长期不予治疗,会造成骨坏死或椎体出现裂缝。椎体压缩性骨折的检测主要是为了减轻椎体塌陷所致的疼痛,快速启动最佳治疗方案,防止相关并发症,以及避免新的骨折。在最近的一项研究中,Wang等证明了双源CTVNC技术可以清晰地显示急性椎体压缩性骨折中的BME,并证实在双源CTVNC图像中有BME组和无BME组的椎体平均CT值之间存在显著差异。
用颜色编码图像和灰阶图像早期诊断椎体压缩性骨折的BME可以帮助制定治疗计划,如哪些患者适合椎体成形术、哪些患者适合禁止运动以防止并发症。在VNC图像中,由于成人大部分腰椎椎体充满了脂肪,所以正常腰椎的平均CT值为负值;而胸椎中黄骨髓和红骨髓之间的比例比较均衡,正常胸椎的平均CT值为正值。骨挫伤及正常的胸椎组与腰椎组的平均CT值之间均存在统计学差异,因此Bierry等计算出了两个不同的可视化临界值(35和6.5)。以MRI作为参考标准,双源CT对BME的视觉分析的总体敏感性及特异性分别为85%和97%。
阴性预测值很高(>97%),说明双源CT可以作为排除近期骨折的潜在重要方法。在形态学未见异常的胸椎和腰椎椎体中阴性预测值仍然很高,因此双源CT可以排除只在MRI上可见的隐匿性骨折。然而,双源CTVNC图像在诊断BME时有一些影响因素。骨折愈合时可引起骨量增多或椎体硬化,骨折椎体出现的裂缝内可见气体或水,而在双源CTVNC图像中椎体内的气体或硬化会使骨髓的衰减度降低(即平均CT值减低)。
椎体内存在气体或硬化会使假阴性率升高。Wang等证实,在椎体内硬化、气体少于50%的患者中,双源CT对椎体压缩性骨折的诊断效果更好,敏感性增高至96%。此外,在骨质疏松患者中,骨小梁的减少及骨密度的减低可能也会改变衰减度。因此,骨质疏松组及非骨质疏松组的VNC图像应该有不同的参数设置。今后我们还需进一步研究不同条件下双源CTVNC技术的最优化参数设置等问题。
综上所述,双源CTVNC技术能够视觉分析及定量分析隐匿性骨折所致BME的衰减变化。此外,由于其在BME检测中具有较高的阴性预测值,能够排除骨质形态学完整的隐匿性骨折,因此可以作为排除急性损伤的一种快速方便的筛查工具。对于可疑急性隐匿性骨折的患者,双源CT将会成为潜在的一站式检查方法,因为CT对于检测骨皮质的中断(显示骨折线)较MRI敏感性更高,而且扫描速度更快。
如果患者具有MRI检查的禁忌症,双源CT能够为患者提供一种替代性的影像学检查。随着双源CT及VNC图像分析软件的广泛应用,其将成为骨及骨髓综合评估的一站式检查方法。双源CTVNC技术的临床应用价值必将在今后的研究中得到证实。预计双源CTVNC将会推出一代又一代能够更好地检测骨髓水肿的新算法,从而降低假阳性率,提高特异性。
来源:中国临床医学影像杂志2016年第27卷第1期
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#隐匿性#
31
#应用进展#
28
#双源CT#
0
很好,不错,以后会多学习
61
很好,不错,以后会多学习
63
很好,不错,以后会多学习
59
#隐匿#
41