Cardiovasc Diabetol:血Asprosin可作为糖尿病患者外周动脉疾病的诊断标志物
2022-02-23 Nebula MedSci原创
循环 Asprosin 水平升高是下肢外周动脉疾病的独立危险因素,可作为诊断标志物
功能失调的脂肪组织中脂肪因子分泌的改变会促进动脉粥样硬化疾病 (包括下肢外周动脉疾病[PAD]) 的发展。Asprosin(白脂素)是最近发现的一种脂肪因子,在新陈代谢中表现出强大的调节作用,但 Asprosin 与下肢外周动脉疾病之间的关系仍未明确。
本研究招募了33位2型糖尿病(T2DM)患者(DM组)、51位有下肢外周动脉疾病的T2DM患者(DM+PAD组)和30位健康对照(NC),采集了所有受试者的血样以进行循环 Asprosin 水平分析和代谢筛查。使用来自 2 型糖尿病 db/db 小鼠的主动脉组织进行 RNA 测序,并用 Asprosin 处理人脐静脉内皮细胞 (HUVEC) 以评估其对内皮-间质转化 (EndMT) 的影响。
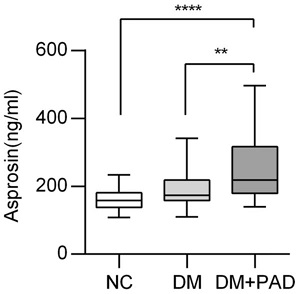
各组的Asprosin水平
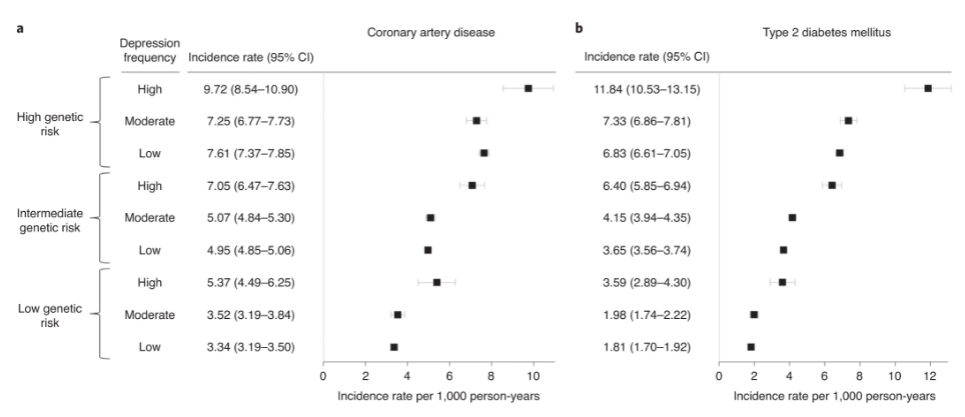
DM+PAD组受试者的 Asprosin 水平明显高于 NC 组和 DM 组。循环 Asprosin 水平与踝臂指数(ABI)呈显著负相关,即使根据年龄、细胞、体重指数(BMI)和 PAD 的其他传统风险因素进行调整后该相关性仍具有显著性。逻辑回归分析显示,Asprosin 是 PAD 的独立危险因素,ROC 曲线显示,Asprosin 具有区分 PAD 的良好敏感性 (74.5%) 和特异性 (74.6%)。
根据Asprosin水平分析的PAD敏感性和特异性
代谢组学数据显示,PAD 患者肌成纤维细胞产生胶原蛋白的过程中氨基酸从头合成具有典型特征,db/db 小鼠的主动脉组织 TGF-β 信号通路被激活。Asprosin 以 TGF-β 依赖性方式直接诱导 HUVECs 中的内皮-间质转化;TGF-β 信号通路抑制剂 SB431542 可消除 Asprosin 对 EndMT 的促进作用。
综上,循环 Asprosin 水平升高是下肢外周动脉疾病的独立危险因素,可作为诊断标志物。从机制上讲,Asprosin 通过激活 TGF-β 信号通路直接诱导内皮-间质转化参与血管损伤。
原始出处:
You, M., Liu, Y., Wang, B. et al. Asprosin induces vascular endothelial-to-mesenchymal transition in diabetic lower extremity peripheral artery disease. Cardiovasc Diabetol 21, 25 (2022). https://doi.org/10.1186/s12933-022-01457-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
39
#DIA#
38
#标志物#
43
#BET#
39
#诊断标志物#
47
#诊断标志#
46
#ROS#
33
#糖尿病患者#
29
#外周动脉#
40
#PRO#
39