Stroke:中国颅内动脉狭窄支架术后30天预后的研究
2015-09-20 MedSci MedSci原创
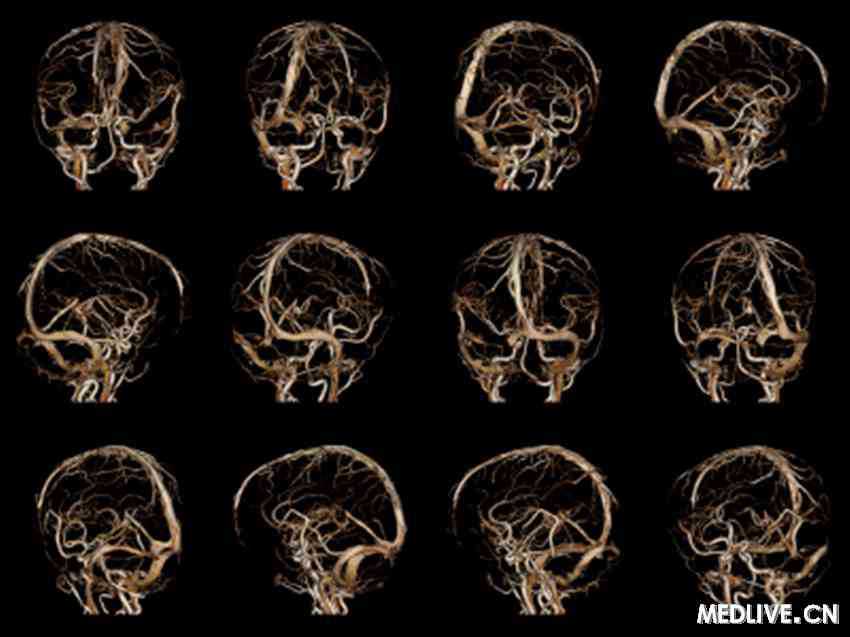
背景和目的:尽管最近试验表明严重症状性颅内动脉粥样硬化性狭窄患者放置支架治疗效果不如药物治疗,但是这个结论是否适用于灌注不足症状的患者尚不清楚。研究人员进行了一项多中心前瞻性研究评估严重症状性颅内动脉粥样硬化性狭窄的患者进行支架术后30天内的安全性和有效性。 方法:招募由于动脉狭窄70%到90%所引起的症状性颅内动脉粥样硬化性狭窄的患者。根据指南手术者放置球囊导管支架或者球囊预扩张后自展式支架给予
背景和目的:尽管最近试验表明严重症状性颅内动脉粥样硬化性狭窄患者放置支架治疗效果不如药物治疗,但是这个结论是否适用于灌注不足症状的患者尚不清楚。研究人员进行了一项多中心前瞻性研究评估严重症状性颅内动脉粥样硬化性狭窄的患者进行支架术后30天内的安全性和有效性。
方法:招募由于动脉狭窄70%到90%所引起的症状性颅内动脉粥样硬化性狭窄的患者。根据指南手术者放置球囊导管支架或者球囊预扩张后自展式支架给予治疗。主要终点为30天内卒中,短暂性脑缺血发作以及死亡。次要终点为成功血管再通。比较两个治疗组患者的基本特征以及预后。
结果:从2013年9月到2015年1月,在354名患者中,招募300名患者(年龄为58.3±9.78岁),159名患者放置球囊导管支架,141名患者球囊扩张后放置自展支架。30天患者卒中,短暂性脑缺血发作以及死亡的发生率为4.3%。成功再通的患者占97.3%。与球囊扩张后置入自展支架的患者相比,放置球囊导管支架的患者年龄较大,大脑中动脉损伤的可能性较小,椎动脉损害的可能性较大,Mori A区损害的可能性较大,Mori C区损害的可能性较小,残余狭窄的水平较低。
结论:严重症状性颅内动脉粥样硬化性狭窄的患者,放置血管支架的短期安全性和有效性尚可。与放置自展支架的患者相比,放置球囊导管支架的患者残余狭窄水平较低。
原文出处:
Miao Z, Zhang Y, Shuai J,et al. Thirty-Day Outcome of a Multicenter Registry Study of Stenting for Symptomatic Intracranial Artery Stenosis in China.Stroke. 2015 Aug 18. pii: STROKEAHA.115.010549. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#30天#
40
#支架术#
33
#支架术后#
28
#颅内动脉狭窄#
30
这篇文章写得很好
138
这篇文章写得很好
109
这篇文章写得很好
109
#动脉狭窄#
28