FDA限制Stryker Wingspan颅内支架系统的使用
2012-08-14 陈蓉 医学论坛网
2012年8月8日,美国食品与药物管理局(FDA)批准Stryker Wingspan颅内支架系统包括适应证在内的标签修改,增加了新的禁忌症、使用警告及对该装置风险的详细描述。 颅内狭窄动脉或阻塞可减少颅内动脉血供,极大增加患者致死性卒中发生风险。对于颅内动脉严重狭窄目前有几种治疗方案可供选择,Wingspan支架系统可用
2012年8月8日,美国食品与药物管理局(FDA)批准Stryker Wingspan颅内支架系统包括适应证在内的标签修改,增加了新的禁忌症、使用警告及对该装置风险的详细描述。
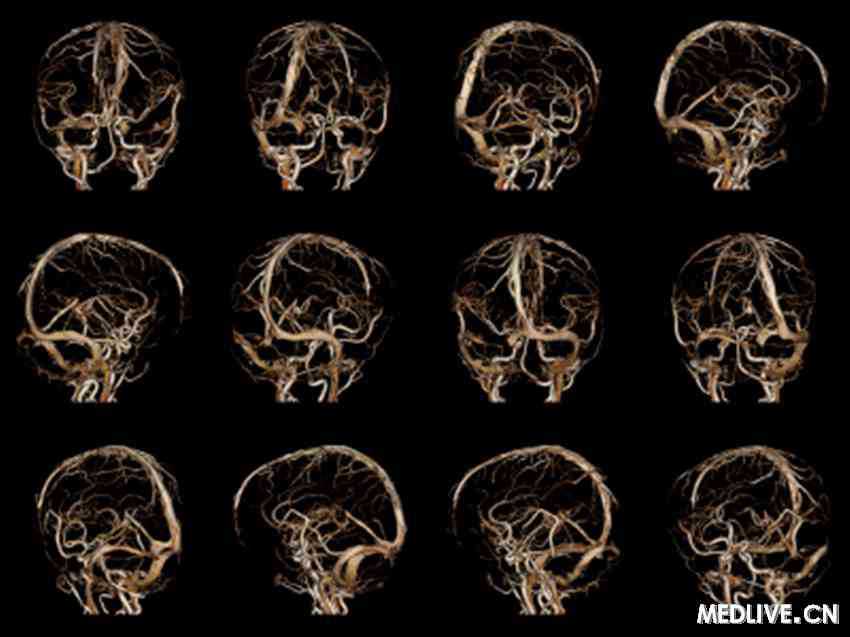
颅内狭窄动脉或阻塞可减少颅内动脉血供,极大增加患者致死性卒中发生风险。对于颅内动脉严重狭窄目前有几种治疗方案可供选择,Wingspan支架系统可用于扩张颅内狭窄动脉而预防新发卒中。
自2005年该系统被批准以来,包括SAMMPRIS(颅内动脉狭窄患者采取支架置入与积极药物治疗预防卒中复发研究)在内的临床试验数据表明,与单纯药物治疗相比,颅内支架置入可能增加部分患者的卒中和死亡风险。然而,入组SAMMPRIS研究的患者与其他试验入组患者有很大差异,这些差异影响了患者的获益和风险。
经过对这些临床试验数据的回顾,FDA认为Wingspan支架系统依旧可以用于有限的患者,尤其是接受药物治疗存在卒中再发,在接受支架置入前7天无新发卒中症状的患者。Stryker将增强对临床医生使用Wingspan支架系统的培训,此外,FDA还要求Stryker提供更多的上市后监督研究数据。
相关链接:FDA revises safety information and limits use of Stryker Wingspan brain stent system,FDA,Aug. 8, 2012
相关链接:FDA revises safety information and limits use of Stryker Wingspan brain stent system,FDA,Aug. 8, 2012
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SpA#
37
#NGS#
46
#GSP#
41