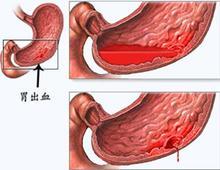
Gastroenterology:质子泵抑制剂的使用与华法林相关上消化道出血风险降低有关
2016-11-30 haofan MedSci原创
对在田纳西州医疗补助计划和5%国家医疗样本两个研究人群开始华法林治疗的患者进行分析,联合PPI治疗与华法林相关的上消化道出血风险降低有关;并且在同时服用抗血小板药物或非甾体类抗炎药的患者中这种风险降低最多。
质子泵抑制剂(PPI)可能会降低华法林相关严重上消化道出血风险,但能证实对这种指征进行PPI治疗具有疗效的证据较为有限。对于服用华法林同时加入抗血小板药物或非选择性非甾体类抗炎药(NSAIDs)的患者,这将进一步增加的胃肠道出血的风险,因此,PPI的胃保护作用对这些患者特别重要。
这项回顾性队列研究在田纳西州医疗补助计划和5%国家的医疗保险样本两个研究人群中开始华法林治疗的患者中进行,并确定了97,430例新发华法林治疗患者,以75,720人/年进行后续随访。该研究的终点为可通过服用PPI来预防的上消化道出血和其他部位出血而住院。
在服用华法林但未联合PPI治疗的患者中,每年每10,000人中就有119人因上消化道出血而住院,而在那些服用华法林联合PPI治疗的患者中因上消化道出血而住院的风险降低了24%(调整后的风险比为0.76;95%可信区间为0.63−0.91),而因消化道其他部位出血而住院(风险比为1.07;95%可信区间为0.94−1.22)和非消化道出血而住院(风险比为0.98;95%可信区间为0.84−1.15)的风险均没有显著降低。同时使用抗血小板药物或非甾体类抗炎药的患者中,那些服用华法林但未联合PPI治疗的患者每年每10,000人中就284人因上消化道出血而接受治疗,而联合PPI治疗的患者风险降低了45%(风险比为0.55;95%可信区间为0.39−0.77)。联合PPI治疗在未使用抗血小板药物或非甾体类抗炎药的华法林患者中无明显的保护作用(风险比为0.86;95%可信区间为0.70−1.06),而且在这两个研究人群中的研究结果相类似。
由此可见,对在田纳西州医疗补助计划和5%国家医疗样本两个研究人群开始华法林治疗的患者进行分析,联合PPI治疗与华法林相关的上消化道出血风险降低有关;并且在同时服用抗血小板药物或非甾体类抗炎药的患者中这种风险降低最多。
原始出处:
Wayne A. Ray, et al. Association of Proton Pump Inhibitors With Reduced Risk of Warfarin-Related Serious Upper Gastrointestinal Bleeding. Gastroenterology .2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#GAS#
27
#AST#
33
#上消化道#
24
#风险降低#
0
#抑制剂#
33
#质子泵#
33
#Gastroenterol#
25
长知识,热点
82
PPI与华法林合用,对血药浓度有没有影响
64
#消化道#
21