JAHA:急性脑出血后心率变异性对结局的影响
2021-08-14 MedSci原创 MedSci原创
急性ICH初始24小时内平均HR和HR-ARV的增加与不良结局独立相关。此外,HR-ARV与24小时血肿扩大相关。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在探讨急性脑出血(ICH)后最初24小时内心率(HR)和心率变异性(HRV)的临床意义,以及如何导致更差的临床结局。
在ATACH-2(脑出血降压治疗2)试验中,在随机分组后的最初24小时内,从基线到1小时每15分钟和每小时记录一次HR。研究人员计算了以下内容:平均值、标准偏差、变异系数、连续变异和平均实际变异(ARV)。结局为24小时血肿扩大和不利的功能结局,定义为90天时改良Rankin量表评分为4至6。
 在ATACH-2试验中的1000名受试者中,994名具有可用HR数据的受试者被纳入分析。总体而言,262例患者出现血肿扩大,362例患者出现不良结局。
在ATACH-2试验中的1000名受试者中,994名具有可用HR数据的受试者被纳入分析。总体而言,262例患者出现血肿扩大,362例患者出现不良结局。
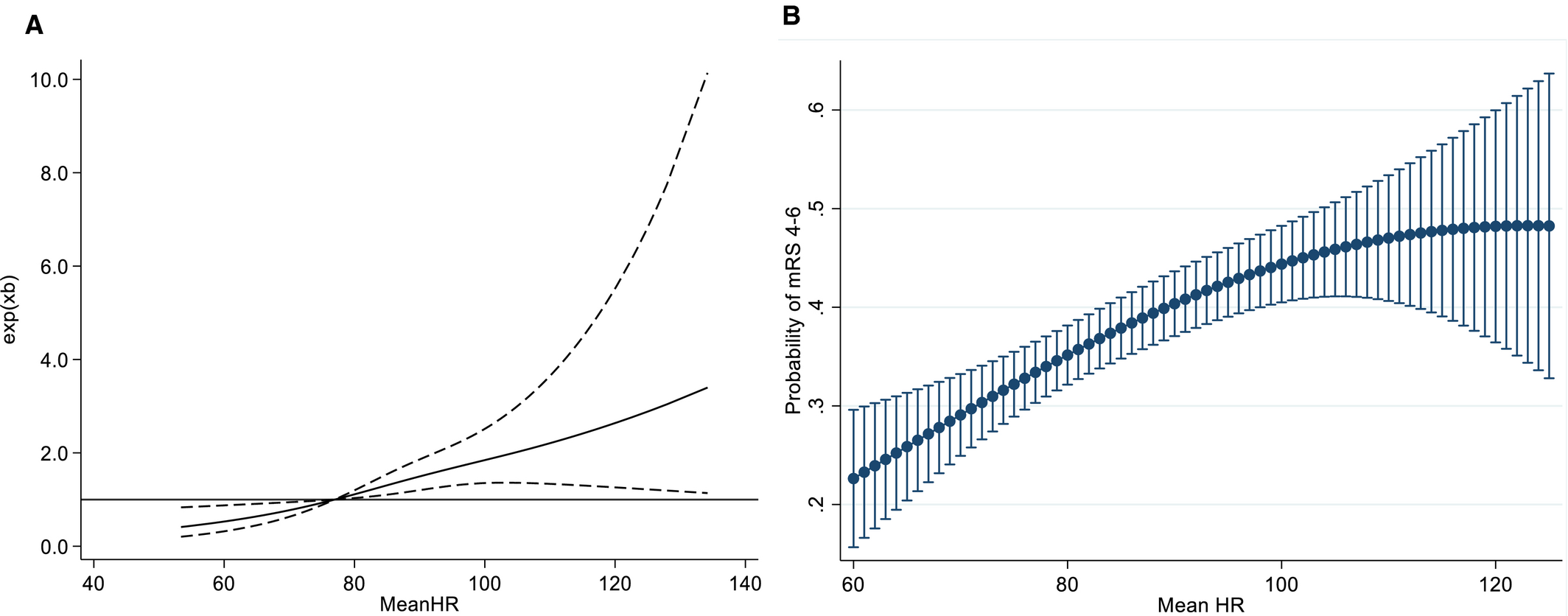
平均心率 (HR) 与不良功能结局之间的关联
平均HR增加与不利结局线性相关(每增加10 bpm调整比值比[aOR]为1.31,95%CI为1.14-1.50),但与血肿扩大无关,而HR-ARV与血肿扩大(aOR为1.06,95%CI为1.01-1.12)和不利结局(aOR为1.07,95%CI为1.01-1.3)相关。平均HR每增加10 bpm,不良结局的发生概率增加4.3%,而HR-ARV每增加1,血肿扩大的发生概率增加1.1%,不良结局的发生概率增加1.3%。
由此可见,急性ICH初始24小时内平均HR和HR-ARV的增加与不良结局独立相关。此外,HR-ARV与24小时血肿扩大相关。
原始出处:
Kaori Miwa.et al.Effect of Heart Rate Variabilities on Outcome After Acute Intracerebral Hemorrhage: A Post Hoc Analysis of ATACH‐2.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.020364
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










受益匪浅
59
#AHA#
36
#变异#
41
#心率变异性#
42
学习了
53
非常棒🌹🌹🌹
66