ERJ:戴智育教授课题组最新研究进展:PHD2缺失诱发肺动脉高压的硝化应激
2022-07-09 刘少飞 MedSci原创
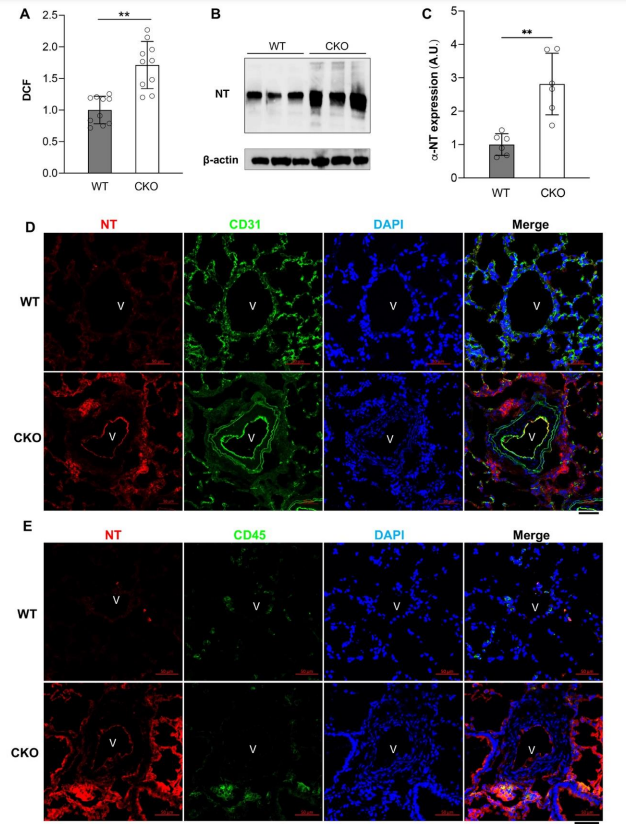
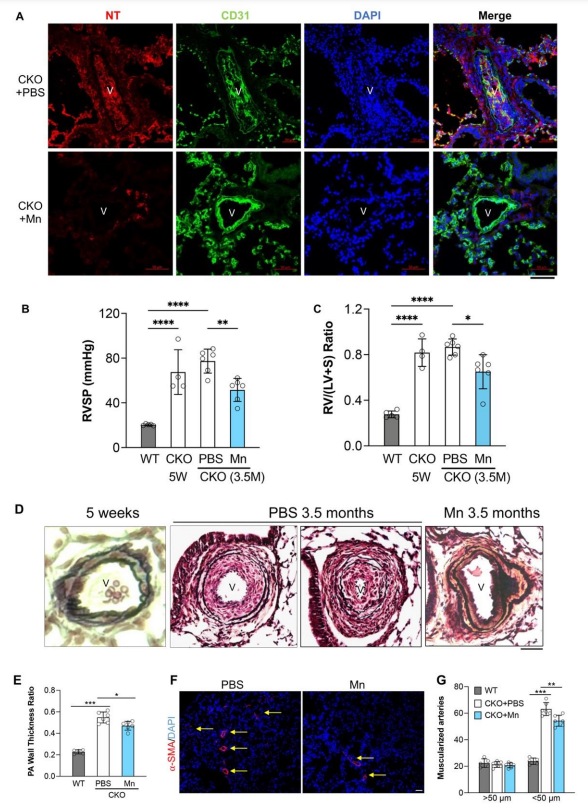
本研究表明,硝化应激在肺部,特别是在CKO小鼠的血管病变中明显增强,再现了临床PAH的病理特征。硝化应激的增加是由于内皮细胞Cav1的缺乏和eNOS的激活。
肺动脉高压(PAH)是一种进展性的心血管疾病,其特点是肺血管阻力持续增加和阻塞性肺血管重塑,从而导致右心衰竭和过早死亡。不同病因引起的PAH的组织病理学特征包括血管壁厚度增加、血管纤维化、氧化/硝化应激增加、微血管闭塞和复杂的丛状病变。鉴于对闭塞性肺血管重塑的分子机制还不完全了解,目前主要针对血管收缩的PAH治疗,对血管重塑影响不大,不能有效地治愈疾病。
研究背景:
越来越多的证据表明特发性PAH(IPAH)患者的肺部存在氧化/硝化应激。在IPAH肺部,参与生成超氧阴离子(活性氧,ROS)的黄嘌呤氧化酶活性明显增加,它们有助于慢性缺氧引起的PH。包括Nox1、2和4在内的NADPH氧化酶也产生大量的ROS,已被证明参与了PH的发展。8-羟基鸟苷(由超氧化物与鸟嘌呤反应引起的氧化损伤的非标记物)染色在IPAH患者丛状病变的内皮细胞(ECs)中非常明显。 相反,抗氧化剂如锰超氧化物歧化酶(MnSOD,一种由SOD2基因编码的关键线粒体抗氧化酶)的活性在IPAH肺部较低。一氧化氮(NO)和超氧化物的过度产生导致了破坏性的过氧亚硝酸盐的形成。过氧亚硝酸盐(即硝化应激)的水平升高是有害的,它诱发了肺血管细胞的细胞损伤和死亡,包括ECs和平滑肌细胞(SMCs)。此外,过氧亚硝酸盐修饰酪氨酸残基,导致蛋白质的酪氨酸硝化(形成3-硝基酪氨酸),从而改变其功能。IPAH患者的肺部过氧亚硝酸盐水平升高,这部分是由于组织缺氧和炎症引起的。免疫组化染色显示3-硝基酪氨酸明显增加。之前的研究表明,Caveolin-1(Cav1)的缺乏导致eNOS的激活和一氧化氮水平的明显增加,以及超氧化物的增加,形成过氧化氢,导致肺血管中突出的硝化压力。
正如在Prkg1 KO (Prkg编码PKG)小鼠中看到的那样,硝化应激的增加导致蛋白激酶G(PKG)的酪氨酸硝化,损害其激酶活性,导致血管收缩和血管重塑的增强,从而导致PH的发生发展。在IPAH患者的肺部,PKG的酪氨酸氮化明显增加。
研究目的:
最近,我们报道了前所未有的严重PH的小鼠模型[Tie2Cre介导的Egln1,编码缺氧诱导因子(HIF)脯氨酰羟化酶2(PHD2),指定为Egln1Tie2Cre,CKO],具有进行性血管重塑,包括血管闭塞和丛状病变以及右心衰竭,这再现了临床PAH包括IPAH的许多特征。
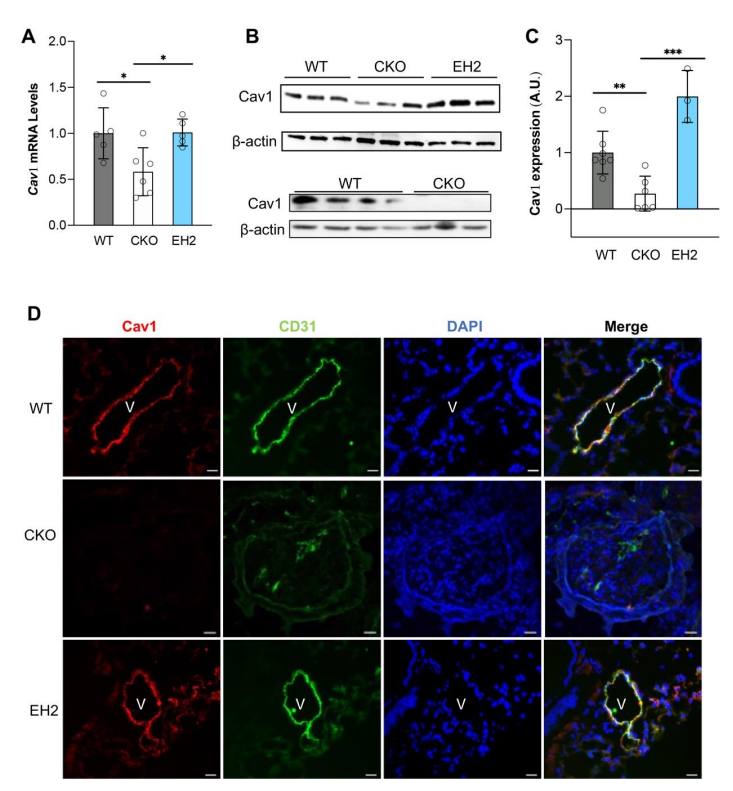
然而,目前还不知道在这种严重的PH模型中,氧化/硝化应激是否也被增强并参与了PH的发病机制。在这种严重的PH模型中参与PH的发病机制。在本研究中,我们首次证明了内皮细胞PHD2的缺失通过下调氧化/硝化应激导致PH。通过下调内皮Cav1的表达,以HIF-2依赖的方式诱导广泛的氧化/硝化压力。ROS清除剂的处理、遗传性中断的 EC特异性Nos3的基因中断或恢复Cav1的表达,明显地减少了硝化应激并减弱了CKO小鼠的PH进展。
研究结果:
1. CKO小鼠肺部和肺血管ECs中突出的硝化应激。
2. 用ROS/过氧亚硝酸盐清除剂MnTMPyP(Mn)处理抑制了CKO小鼠的血管进行性重塑并减轻了PH。
3. 敲除ECs的Nos3后,减少了CKO小鼠的硝化应激、血管重塑和严重的PH。
4
4. 内皮细胞Cav1的表达在CKO小鼠肺部以HIF-2α依赖性的方式被抑制。
5. 在CKO小鼠中Cav1的转基因表达。

6. Cav1转基因表达抑制了CKO小鼠肺部过多的ROS/RNS表达
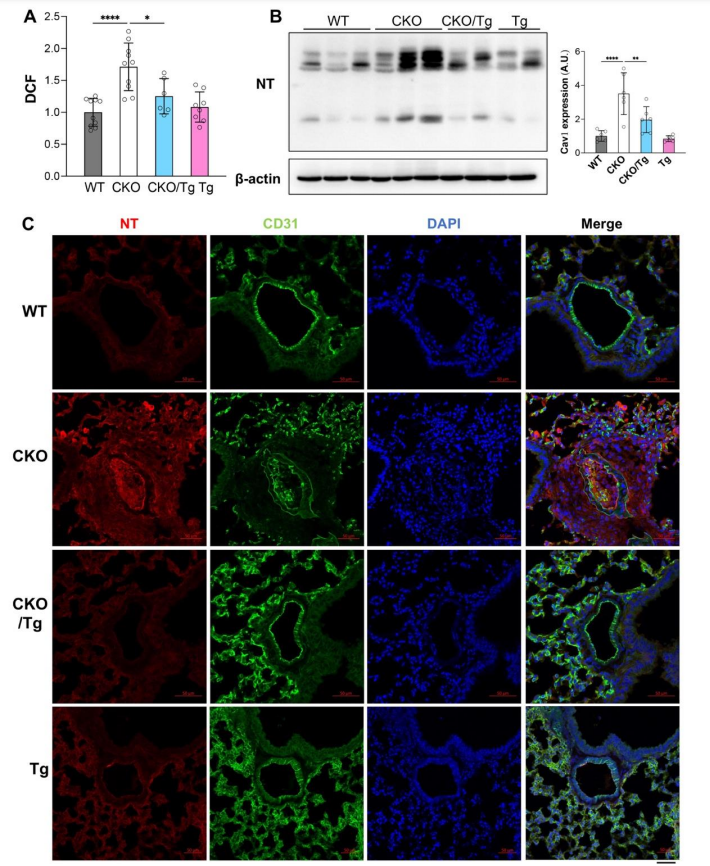
7. Cav1的转基因表达抑制了CKO小鼠的严重PH。
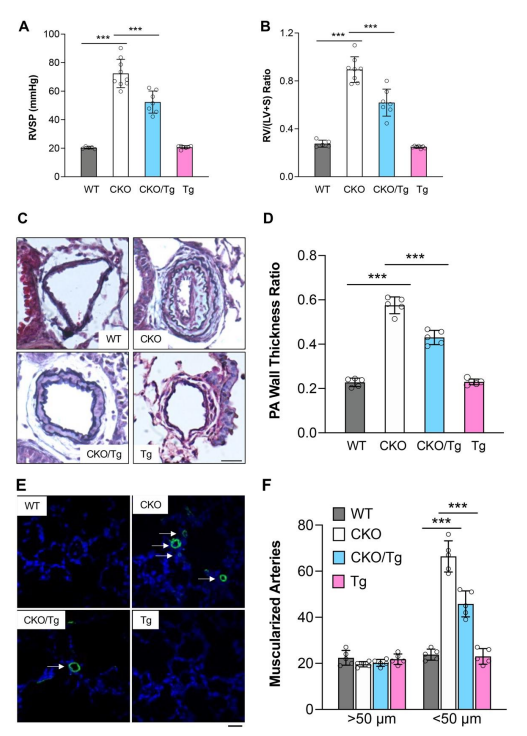
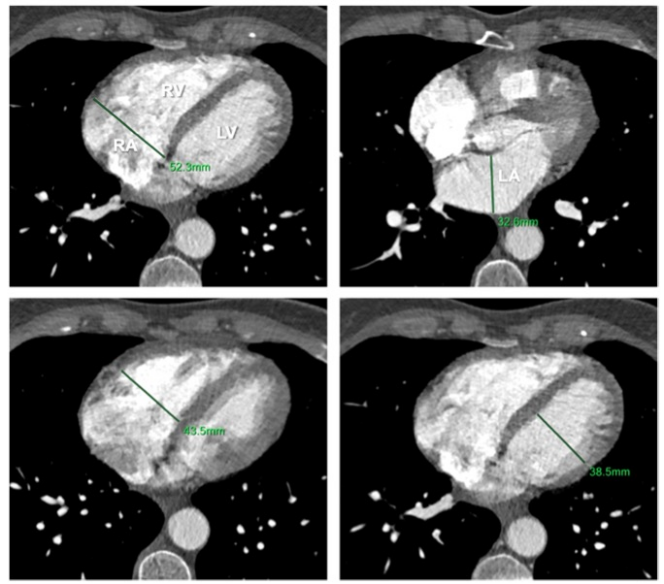
8. Cav1的转基因表达改善了Egln1Tie2Cre/Cav1Tg小鼠的右心和肺动脉功能。

本研究表明,硝化应激在肺部,特别是在CKO小鼠的血管病变中明显增强,再现了临床PAH的病理特征。硝化应激的增加是由于内皮细胞Cav1的缺乏和eNOS的激活。Cav1在CKO/Tg小鼠中的转基因表达降低了硝化应激水平,并通过减少RVSP、肺血管重塑和RV肥大,以及改善RV和PA 功能。药物清除ROS/RNS和通过CRISPR-Cas9技术的EC靶向纳米粒子传递对成年小鼠内皮Nos3的基因敲除都减少了硝化应激,并明显降低了CKO小鼠肺血管重塑和PH的严重程度。这些发现表明,恢复Cav1的表达和清除ROS/RNS是治疗严重PAH的潜在策略。治疗严重PAH,包括IPAH(图8F)。我们以前观察到IPAH患者闭塞性肺血管的ECs中PHD2的表达减少,这也验证了其临床意义。
参考文献:
Liu B, Peng Y, Yi D, Machireddy N, Dong D, Ramirez K, Dai J, Vanderpool R, Zhu MM, Dai Z, Zhao YY. Endothelial PHD2 deficiency induces nitrative stress via suppression of caveolin-1 in pulmonary hypertension. Eur Respir J. 2022 Jul 7:2102643. doi: 10.1183/13993003.02643-2021. Epub ahead of print. PMID: 35798360.
本文作者:
戴智育博士致力于血管生物学研究,在肺血管疾病致病机制以及小分子基因治疗靶点的转化与开发等领域有着深厚的造诣和突出的成绩,发表了包括Circulation等杂志在内的多篇高水平论文和研究成果。其首次提出的Egln1Tie基因(编码PDH2)敲除小鼠模型可再现肺动脉高压肺血管重构的临床表型,突破了肺动脉高压研究领域中,疾病实验动物模型与疾病临床表型不相匹配的难题。此外,在该Egln1Tie基因敲除小鼠模型中共同敲除Hif-2α基因可加重肺血管重构,其主要机制可能是通过激活基质细胞衍生因子-1(CXCL12)发挥作用,敲除Cxcl12基因可改善Egln1Tie基因敲除小鼠模型的肺血管病变程度。因此,靶向PHD2/HIF2α信号途径是未来具有前途的逆转肺血管重构的基因治疗方案之一。
实验室网站(常年接收PhD及博士后,访问学者申请):
https://cts.uahs.arizona.edu/people/zhiyu-dai

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#最新#
37
#PhD#
27
#动脉高压#
28
#研究进展#
45
#应激#
44
#PHD2#
46
精彩评论,需要您登录查看
43