European Radiology:CTPA自动心室三维容积法在诊断左心源性肺动脉高压方面的准确性
2022-07-06 shaosai MedSci原创
CT肺血管造影(CTPA)是怀疑有PH患者排除肺栓塞和肺实质疾病的首选影像学检查。
 肺动脉高压(PH)是一种血流动力学状态,定义为通过右心导管检查(RHC)测得的静止状态下平均肺动脉压(mPAP)的病理性升高。世界卫生组织(WHO)的PH分类根据病因、血流动力学特征、临床结果和治疗策略的相似性区分为五组。在血液动力学上,PH可细分为毛细血管前、毛细血管后或合并毛细血管前和毛细血管后的PH。
肺动脉高压(PH)是一种血流动力学状态,定义为通过右心导管检查(RHC)测得的静止状态下平均肺动脉压(mPAP)的病理性升高。世界卫生组织(WHO)的PH分类根据病因、血流动力学特征、临床结果和治疗策略的相似性区分为五组。在血液动力学上,PH可细分为毛细血管前、毛细血管后或合并毛细血管前和毛细血管后的PH。
左心病引起的PH(WHO第2组PH)是毛细血管后PH的一种形式,是左心病(LHD)的常见并发症,与预后恶化相关。其诊断主要是通过RHC测量的静止状态下肺动脉楔压(PAWP)升高>15毫米汞柱来定义。然而指南建议,在有创导管检查之前应根据非侵入性参数估计LHD的临床试验前概率以改善第2组PH与其他原因的区分,并改善有创左右心导管检查的指示。
CT肺血管造影(CTPA)是怀疑有PH患者排除肺栓塞和肺实质疾病的首选影像学检查。研究表明,CTPA上测量的左心房直径和面积增大对识别第2组PH具有良好的诊断准确性。然而,心腔容积测量法在检测心腔扩大方面可能更加准确和可靠。据我们所知,只有少数研究调查了心腔容积区分第2组PH和其他原因的能力,且未与同一患者群中的人工直径测量进行比较。
近日,发表在European Radiology杂志的一项研究评估了基于CTPA的心腔自动三维容积测量对WHO第2组PH的诊断准确性以及与其他PH组(非第2组PH)之间的鉴别,为PH的准确诊断及分型提供了技术支持。
本研究在2013年8月至2016年2月期间对100天内接受右心导管检查和CTPA诊断的确诊PH患者进行了评估。两个放射科医生使用商业软件对左心房、左心室、右心房和右心室(LA/LV/RA/RV)进行了自动三维分割。通过逻辑回归的方式评估区分第2组PH和非第2组PH的能力。
共91名患者(中位数67.5岁,44名女性)被纳入研究,其中19名患者(20.9%)被归类为第2组PH。调整年龄、性别和平均肺动脉压后,第2组PH与较大的LA容积(p < 0.001)、较大的LV容积(p = 0.001)、较低的RV/LV容积比(p = 0.04)和较低的RV/LA容积比(p = 0.003)显著相关。LA容积对识别第2组PH表现出最高的鉴别能力(AUC,0.908;95%置信区间,0.835-0.981),并明显优于LA直径(p = 0.009)。所有容积测量的观察者内部和观察者之间的一致性都很好(类内相关系数为0.926-0.999,所有的P<0.001)。
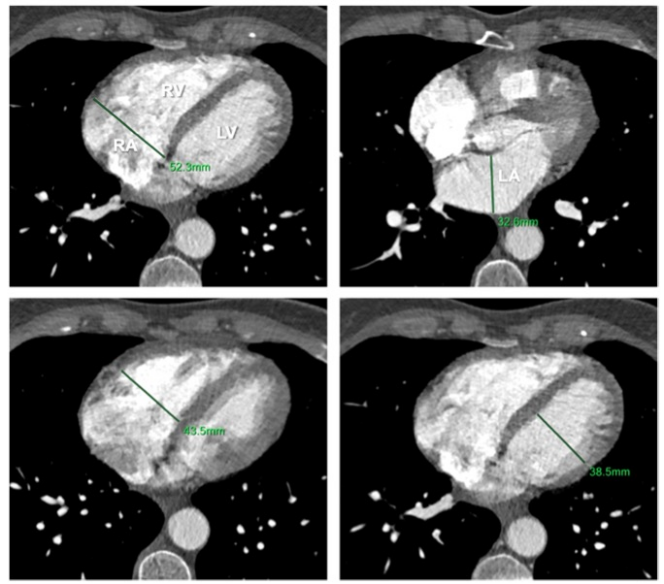
图 在标准轴位CTPA图像上手动测量心腔直径的示例。LA:左心房;LV:左心室;RA:右心房;RV:右心室
本研究表明,基于非门控CTPA的心腔自动三维容积测定可以将WHO第2组PH患者与其他PH组区分开来,且具有良好的诊断准确性。LA容积产生的诊断准确性明显高于CTPA轴位测量的LA直径,可以改善LHD引起的PH的无创分类、从而优化诊断途径。
原文出处:
Claudius Melzig,Thuy Duong Do,Benjamin Egenlauf,et al.Diagnostic accuracy of automated 3D volumetry of cardiac chambers by CT pulmonary angiography for identification of pulmonary hypertension due to left heart disease.DOI:10.1007/s00330-022-08663-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CTP#
52
#tPA#
51
#PE#
48
#动脉高压#
49
#准确性#
69
#心源性#
44
#CTPA#
38