Alzheimer Dementia:血浆置换加白蛋白明显改善老年痴呆患者记忆力和生活质量!
2021-11-07 MedSci原创 MedSci原创
PE治疗的AD患者在记忆力、语言能力、处理速度和QoL-AD方面都有改善。
阿尔茨海默病(AD)的特点是脑损伤和神经元丧失,导致偶发性记忆丧失以及其他认知障碍,包括注意力、注意力、视觉空间能力、心理处理速度、执行功能、言语流畅性以及言语和语言技能方面的缺陷。
随着AD的发展,这些认知症状的恶化在严重程度和频率方面都会加快,这可能导致患者、护理人员和家庭成员被社会排斥,生活质量下降。现有批准的AD治疗方法是对症的,旨在通过调节神经传递--NMDA受体拮抗剂来暂时减缓症状的发展。
近期,来自西班牙记忆诊所的专家开展了一项研究,报告了血浆置换(PE)与白蛋白置换对轻度至中度阿尔茨海默病(AD)患者的神经心理学、神经精神学和生活质量(QoL)结果的影响,这是一项2b/3期试验(阿尔茨海默病白蛋白置换管理[AMBAR]研究)。结果发表在Alzheimer Dementia杂志上。
347名患者被随机分为安慰剂(假PE)和三个PE治疗组,分别使用低/高剂量的白蛋白,同时/不使用静脉注射免疫球蛋白(IVIG)。在基线、第2个月(每周一次的常规PE)、第6、9和12个月(每月一次的低容量PE[LVPE])和第1个月进行具体的测试测量。
结果显示,在第14个月时,经PE治疗的轻度AD患者的语言流畅性和处理速度较安慰剂有所提高(效果大小:>100%;P值:0.03-0.001)。中度AD队列明显改善了短期言语记忆(效果大小:94%->100%;P值:0.02-0.003)。PE治疗的神经精神症状的进展与安慰剂相似。轻度AD患者的QoL有所改善(P值:0.04-0.008)。
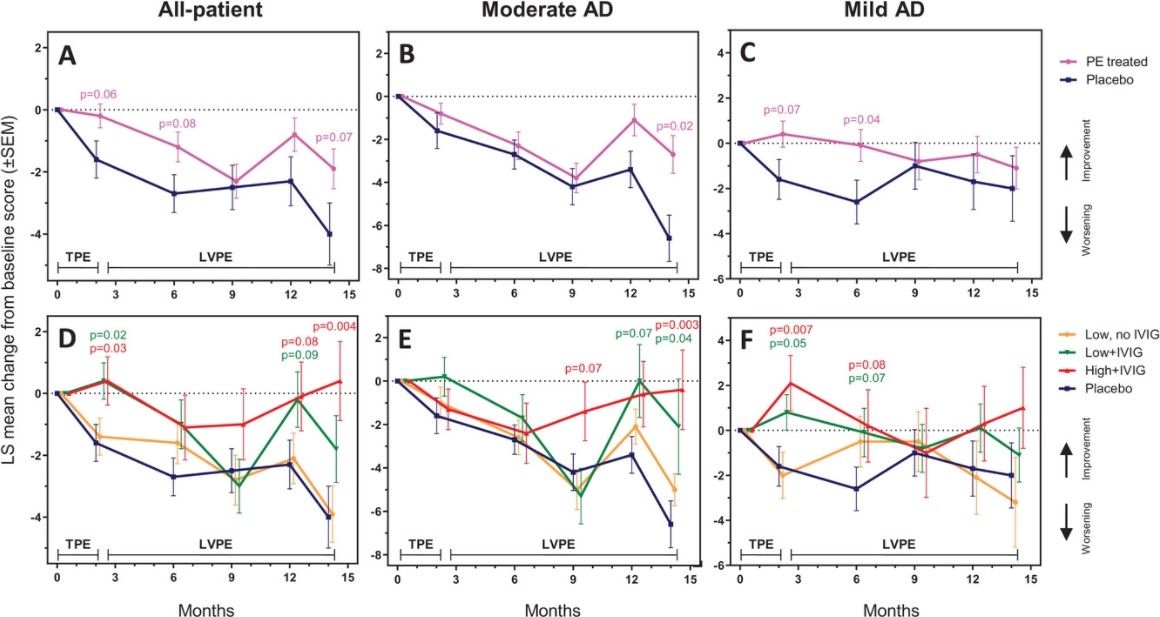
AD患者的Rey听觉言语学习测试得分变化
综上,PE治疗的AD患者在记忆力、语言能力、处理速度和QoL-AD方面都有改善。但并没有观察到他们的心理情感状态的恶化。
参考文献:
Neuropsychological, neuropsychiatric, and quality-of-life assessments in Alzheimer's disease patients treated with plasma exchange with albumin replacement from the randomized AMBAR study. https://doi.org/10.1002/alz.12477
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#dementia#
37
#痴呆患者#
33
#置换#
29
#白蛋白#
39
#血浆置换#
33
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
24