Alz Res Therapy:白质高信号和痴呆影像指标,关系千丝万缕
2021-11-05 Freeman MedSci原创
该结果强调了WMH的模式特异性分布模式,这些模式在后部白质中汇聚。
白质高信号(WMH),使用(FLAIR)磁共振成像(MRI)进行量化,被认为是脑血管疾病的一个标志,与年龄和心血管危险因素密切相关。WMH的存在也与较低的认知能力和临床阿尔茨海默病(AD)的风险增加有关,这表明WM损伤参与了AD的发病机制。
以前的研究表明,使用敏感PET、脑脊液(CSF)或磁共振成像(MRI)生物标志物测量,WM病理学可能与β-淀粉样蛋白(Aβ)斑块、tau缠结和神经变性的病理标志物直接相关。因此,在一些横断面研究中,WMH的更大存在和延伸与更大的Aβ沉积有关,尽管没有一致的发现,以及在通常受AD影响的脑区,葡萄糖代谢更低,灰质体积(GMV)减少。同时,tau病理与全球(全脑)或区域WMH的关系并不一致,一些作者报告了影响,而其他作者没有发现。
在现有的文献中,全局WMH描述符经常被用来量化WM病理学,并评估其与AD的大脑生物标志物的关系。这种方法掩盖了特定区域的影响。因此,最近使用了voxel-wise mapping 方法来确定与Aβ和/或tau负担有关的WM病变的分布模式。这些独立的队列研究结果为脑室周围后部区域参与Aβ沉积和区域WMH之间的关联提供了一致的支持,而这一点在Tau负担中并没有看到。同样,最近的一项研究表明,在Aβ沉积异常的个体中,WM后部的改变(由平均弥散率和WMH评估)在整个生命周期内随年龄而增加。
藉此,德国柏林大学的Malo Gaubert等人,研究了WMH的空间分布,即使用感兴趣区域(ROI)和体素水平的方法来确定,与新皮质Aβ负担、颞-顶叶代谢低下和内侧-颞GMV减少之间的联系。
共155名参与者(IMAP+队列),从正常认知到AD痴呆,获得FLAIR MRI、AV45-PET、FDG-PET和T1 MRI。从FLAIR图像中自动分割出WMH。使用已建立的AD元特征模板从处理过的图像中提取新皮质Aβ沉积(AV45-PET)、颞顶葡萄糖代谢(FDG-PET)和内侧-颞部灰质体积(GMV)的平均水平。在调整了年龄、性别、教育和收缩压的情况下,研究了AD大脑生物标志物和WMH之间的关系,按兴趣区域和体素评估。
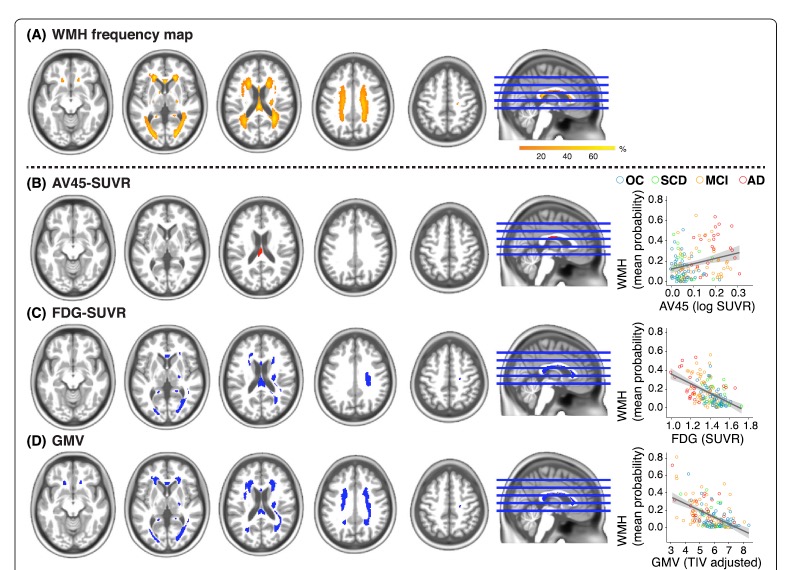 他们发现:全局的Aβ负担和特定区域的WMH之间没有明显的联系。胼胝体中的体素WMH和阈值下更大的Aβ沉积有关。胼胝体后部以及顶叶、枕叶和额叶区域基于区域和体素的WMH与颞顶叶的葡萄糖代谢降低有关。
他们发现:全局的Aβ负担和特定区域的WMH之间没有明显的联系。胼胝体中的体素WMH和阈值下更大的Aβ沉积有关。胼胝体后部以及顶叶、枕叶和额叶区域基于区域和体素的WMH与颞顶叶的葡萄糖代谢降低有关。
同样,内侧-颞侧GMV的降低与胼胝体后部的WMH以及顶叶、枕叶和额叶区域的WMH相关。
这项研究表明,局部白质损伤与AD的多模式大脑生物标志物相关。该结果强调了WMH的模式特异性分布模式,这些模式在后部白质中汇聚。这些横断面研究结果证实了区域性WMH与AD典型的Aβ沉积和神经变性的关联。
原文出处:
Gaubert M, Lange C, Garnier-Crussard A, et al. Topographic patterns of white matter hyperintensities are associated with multimodal neuroimaging biomarkers of Alzheimer’s disease. Alz Res Therapy. 2021;13(1):29. doi:10.1186/s13195-020-00759-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#ERA#
43
#高信号#
48
#白质#
32
#白质高信号#
36
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
33