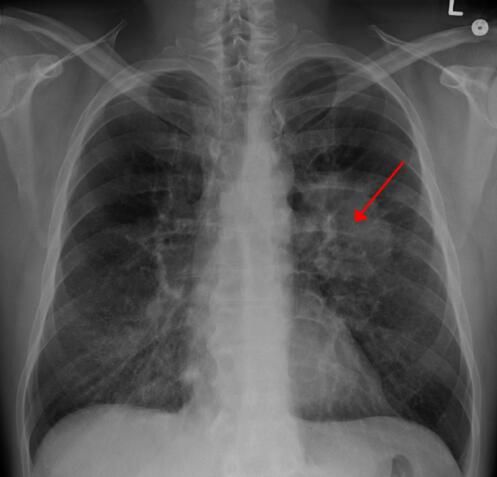
Eur Radiol:FDG-PET/MRI联合DWI检出头颈部鳞状细胞癌放化疗后局部复发的价值
2017-08-26 shaosai MedSci原创
鳞状细胞癌(squamous cell carcinoma)简称鳞癌,为第2个最常见的皮肤恶性肿瘤,起源于皮肤表皮及其附属器(毛囊漏斗、皮脂腺导管、末端汗管) 角质形成细胞,好发于头皮、面部、颈和手背等暴露部位。早期即可呈溃疡,又常继发于慢性溃疡或慢性窦道开口,或瘢痕部的溃疡经久不愈而癌变。临床可呈菜花状,边缘隆起不规则,底部不平,易出血,常伴感染致恶臭。可有局部浸润及区域淋巴结转移。本研究旨在验
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
25
#PE#
39
#PET/MRI#
36
#局部复发#
41
学习并分享!!
59
学习过了.谢谢分享!
70
#放化疗#
23
#DWI#
26
#头颈部鳞状细胞癌#
39
#局部#
24