Eur Heart J:纯合子家族性高胆固醇血症临床管理指南
2014-07-28 cath 编译 医学论坛网
近日,欧洲动脉粥样硬化学会(EAS)发布了纯合子家族性高胆固醇血症(HoFH)临床管理指南,全文7月22日在线发表于《欧洲心脏杂志》(Eur Heart J)。以下为指南摘要内容。 诊断 指南建议, HoFH的早期诊断并及时启动饮食和降脂治疗至关重要。基因学检测可确诊,但如果不可用,低密度脂蛋白胆固醇(LDL-C)显著升高和<10岁出现皮肤或肌腱黄色瘤,或者未经处理的LDL-C水平升高伴有父母
近日,欧洲动脉粥样硬化学会(EAS)发布了纯合子家族性高胆固醇血症(HoFH)临床管理指南,全文7月22日在线发表于《欧洲心脏杂志》(Eur Heart J)。以下为指南摘要内容。
诊断
指南建议, HoFH的早期诊断并及时启动饮食和降脂治疗至关重要。基因学检测可确诊,但如果不可用,低密度脂蛋白胆固醇(LDL-C)显著升高和<10岁出现皮肤或肌腱黄色瘤,或者未经处理的LDL-C水平升高伴有父母患有杂合子FH也提示患者有HoFH。

治疗
指南推荐,疑为HoFH的患者应及时就诊于专科医师,以综合评估动脉粥样硬化性心血管疾病(ACVD)并进行临床管理。生活方式干预和最大量他汀类药物是治疗主要手段,理想治疗时间是于出生后第一年或初次确诊时,常与依折麦布和其他降脂治疗方法联用。
因患者LDL-C很少能达标,如果可以,推荐辅助脂蛋白单采,最好是于患者5岁时启动,不晚于8岁。Lomitapide和mipomersen可作为新的治疗方法使用。
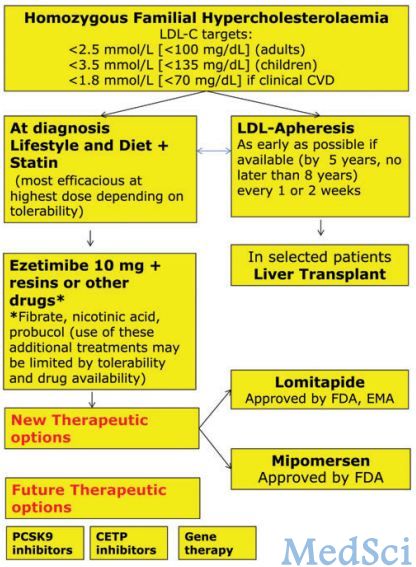
HoFH治疗方案流程图
随访
鉴于ACVD的严重性,指南推荐常规随访,包括每年进行多普勒超声心动图检查和主动脉检查以及压力测试,如果可以,每5年进行CT冠状动脉造影检查,或如有必要此年限可更短。
原始出处:
Cuchel M1, Bruckert E2, Ginsberg HN2, Raal FJ2, Santos RD2, Hegele RA2, Kuivenhoven JA2, Nordestgaard BG2, Descamps OS2, Steinhagen-Thiessen E2, Tybjærg-Hansen A2, Watts GF2, Averna M2, Boileau C2, Borén J2, Catapano AL2, Defesche JC2, Hovingh GK2, Humphries SE2, Kovanen PT2, Masana L2, Pajukanta P2, Parhofer KG2, Ray KK2, Stalenhoef AF2, Stroes E2, Taskinen MR2, Wiegman A2, Wiklund O2, Chapman MJ2; for the European Atherosclerosis Society Consensus Panel on Familial Hypercholesterolaemia.Homozygous familial hypercholesterolaemia: new insights and guidance for clinicians to improve detection and clinical management. A position paper from the Consensus Panel on Familial Hypercholesterolaemia of the European Atherosclerosis Society.Eur Heart J. 2014 Jul 22. pii: ehu274. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#管理指南#
33
#ART#
38
#高胆固醇血症#
44
#临床管理#
38
#HEART#
31
#家族性#
39