Arch Neurol:抗氧化治疗或对阿尔茨海默病无效
2012-03-23 MedSci MedSci原创
3月19日,国际杂志Archives of Neurology在线刊登的一篇研究表明,联合抗氧化治疗并不能改变阿尔茨海默病(AD)患者脑脊液中病理相关标志物水平。 研究显示在对轻中度AD患者使用维生素E、维生素C 和α硫辛酸(ALA)联合抗氧化治疗16周后,其淀粉样蛋白和tau蛋白相关的脑脊液标志物并没有改变,MMSE量表结果显示认知功能呈恶化趋势,但脑脊液中F2-isoprostane(脑
3月19日,国际杂志Archives of Neurology在线刊登的一篇研究表明,联合抗氧化治疗并不能改变阿尔茨海默病(AD)患者脑脊液中病理相关标志物水平。
研究显示在对轻中度AD患者使用维生素E、维生素C 和α硫辛酸(ALA)联合抗氧化治疗16周后,其淀粉样蛋白和tau蛋白相关的脑脊液标志物并没有改变,MMSE量表结果显示认知功能呈恶化趋势,但脑脊液中F2-isoprostane(脑内氧化应激水平的标志)水平显示轻度下降。研究同时显示大剂量辅酶Q10(CoQ)对于改善CSF标志物也没有任何益处。
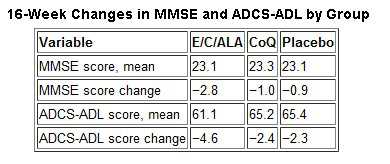
试验随机给予AD患者3种治疗中的1种:800IU/天维生素E+500mg/天维生素C+900mg/天ALA (E/C/ALA)或400 mgCoQ,一天三次或安慰剂治疗。治疗16周后发现与对照组相比,两个药物治疗组患者MMSE及ADCS-ADL分数均有下降。其中66例患者在治疗结束后检测了脑脊液中Aβ42,tau以及P-tau181蛋白的水平,表明联合抗氧化治疗并不影响淀粉样蛋白和tau蛋白病理相关的通路。
研究者推测这种改变提示AD患者的认知功能下降有可能并不是由于AD相关病理标志物的恶化而致,关于其详细机制需要更长期的研究。同时研究者表示,尽管该实验为阴性结果,但有实际的临床意义,至少该研究在验证AD患者给予抗氧化药物治疗是否能够达到真正的预期效果方面是一个尝试。该研究结果不支持辅酶Q10作为进一步治疗AD药物的临床研究。
Douglas R. Galasko, MD; Elaine Peskind, MD; Christopher M. Clark, MD; Joseph F. Quinn, MD; John M. Ringman, MD; Gregory A. Jicha, MD, PhD; Carl Cotman, PhD; Barbara Cottrell, BS; Thomas J. Montine, MD, PhD; Ronald G. Thomas, PhD; Paul Aisen, MD; for the Alzheimer's Disease Cooperative Study
Objective To evaluate whether antioxidant supplements presumed to target specific cellular compartments affected cerebrospinal fluid (CSF) biomarkers.
Design Double-blind, placebo-controlled clinical trial.
Setting Academic medical centers.
Participants Subjects with mild to moderate Alzheimer disease.
Intervention Random assignment to treatment for 16 weeks with 800 IU/d of vitamin E (α-tocopherol) plus 500 mg/d of vitamin C plus 900 mg/d of α-lipoic acid (E/C/ALA); 400 mg of coenzyme Q 3 times/d; or placebo.
Main Outcome Measures Changes from baseline to 16 weeks in CSF biomarkers related to Alzheimer disease and oxidative stress, cognition (Mini-Mental State Examination), and function (Alzheimer's Disease Cooperative Study Activities of Daily Living Scale).
Results Seventy-eight subjects were randomized; 66 provided serial CSF specimens adequate for biochemical analyses. Study drugs were well tolerated, but accelerated decline in Mini-Mental State Examination scores occurred in the E/C/ALA group, a potential safety concern. Changes in CSF Aβ42, tau, and P-tau181 levels did not differ between the 3 groups. Cerebrospinal fluid F2-isoprostane levels, an oxidative stress biomarker, decreased on average by 19% from baseline to week 16 in the E/C/ALA group but were unchanged in the other groups.
Conclusions Antioxidants did not influence CSF biomarkers related to amyloid or tau pathology. Lowering of CSF F2-isoprostane levels in the E/C/ALA group suggests reduction of oxidative stress in the brain. However, this treatment raised the caution of faster cognitive decline, which would need careful assessment if longer-term clinical trials are conducted.
Trial Registration clinicaltrials.gov Identifier: NCT00117403
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阿尔茨#
48
#阿尔茨海#
53
#Neurol#
44
#阿尔茨海默#
62